Unit 1 - Dysphagia
1.2.6. Medical and surgical treatment
In order to diagnose and treat swallowing difficulties, a complete medical history and a thorough physical examination are required. A physical examination of the neck, mouth, oropharynx, and larynx should be conducted, as well as a neurologic evaluation.
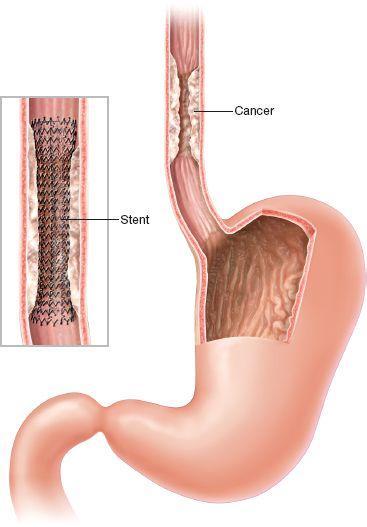
Algorithm for oropharyngeal dysphagia treatment:
Oral phase:
-
Hygiene (For dysphagia patients, oral care entails not just cleaning the mouth, but also avoiding aspiration pneumonia, which can be fatal)

-
Motor/sensorial stimulation; Castillo Morales' orofacial regulation therapy, which combines body and orofacial management with the insertion of a palatal plate, has shown encouraging outcomes in dysphagia patients.
-
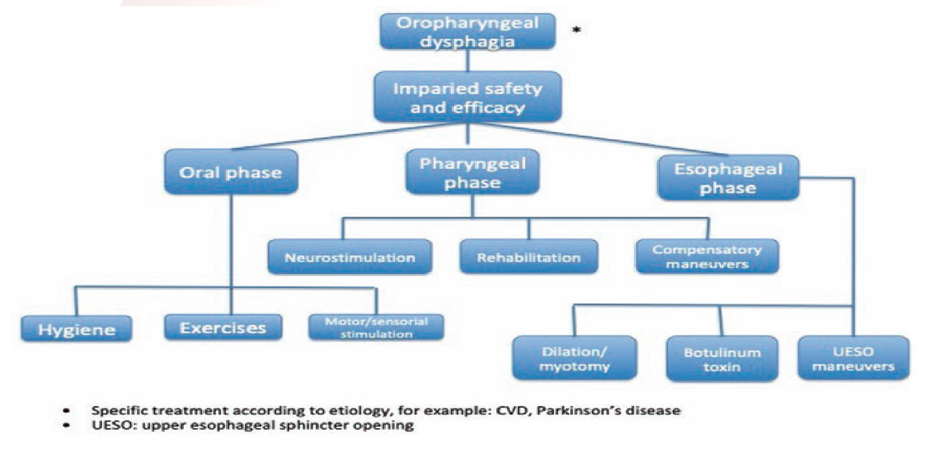
Exercises; Dysphagia patients should begin with exercises like the ones described below, under the supervision of a medical expert such as a speech-language pathologist or an occupational therapist.
(Source: https://www.istockphoto.com)
(Source: obtained from Canva Pro)
Pharyngeal phase:
-
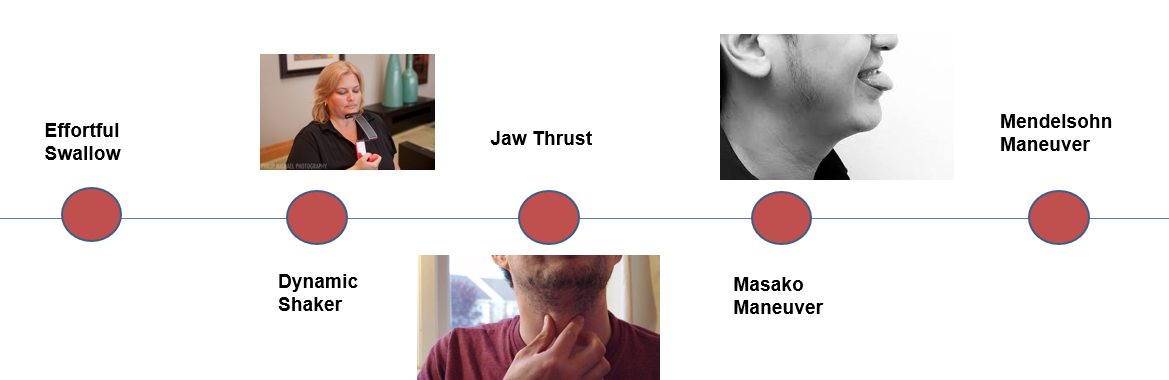
Neurostimulation; Neuromuscular electrical stimulation (NMES) is a type of transcutaneous stimulation that activates sensory or motor nerve fibers involved in swallowing. This mechanism of action is thought to include increasing central nervous system recuperation and speeding up the development of muscle strength.
(Source: obtained from Canva Pro)
-
Rehabilitation; Exercises for swallowing rehabilitation are designed to target certain muscles or muscle groups. Much of today's treatment focuses solely on strength, with little evidence-based studies demonstrating the therapeutic benefits of therapeutic exercises.

-
Compensatory maneuvers; When compensatory techniques are adopted, they alter the swallow but do not result in long-term functional changes. A head rotation, which is utilized during the swallow to steer the bolus toward one of the lateral channels of the pharyngeal canal, is an example of a compensating method.
(Source: https://www.istockphoto.com)
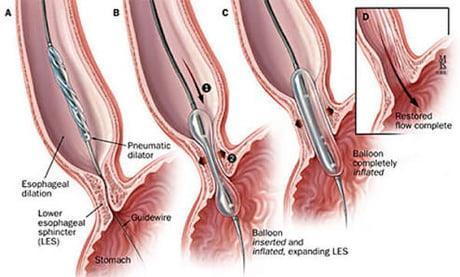
Esophageal phase:
-
Dilation/myotomy; Myotomy can be done through the skin or with an endoscope. Hemorrhage, recurrent laryngeal nerve damage, and pharyngeal or esophageal fistulization are all complications of myotomy.
-
Botolinium toxin; In individuals with OD, BoTox injection might be utilized as the first treatment option. It is simple and safe, and it relieves dysphagia in 43% of instances. Patients with preserved mouth and tongue activity at VFS and intact bolus propulsion capacity on manometry can be offered CP myotomy if BoTox fails.
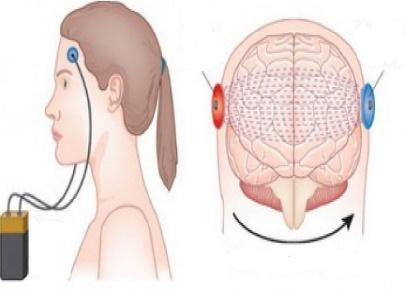
Surgical treatment of OD. Surgery may be indicated to treat esophageal cancer or to improve swallowing problems caused by throat narrowing or obstructions, such as bony outgrowths, vocal cord paralysis, pharyngoesophageal diverticulum, GERD, and achalasia. Following surgery, speech and swallowing treatment is frequently beneficial.
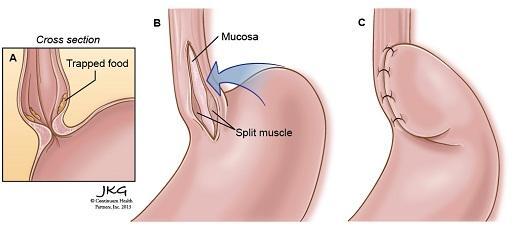
The type of surgical treatment depends on the cause for dysphagia. Some examples are:
- Laparoscopic Heller myotomy - when the muscle at the lower end of the esophagus (sphincter) fails to open and release food into the stomach in persons with achalasia,
this procedure is used to sever it.
-
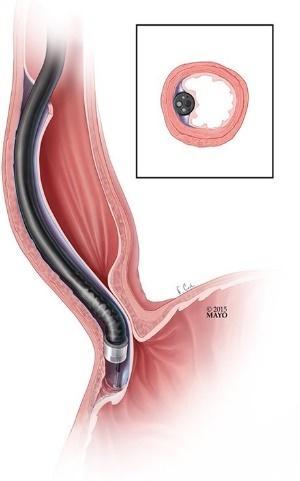
Peroral endoscopic myotomy (POEM) - an endoscope is put into your mouth and down your throat by the surgeon to make an incision in the lining of your esophagus. The surgeon next cuts the muscle at the lower end of the esophageal sphincter, similar to a Heller myotomy.
-
Stent placement - a metal or plastic tube (stent) can also be inserted by your doctor to prop open a narrowing or obstruction in your esophagus. Some stents are permanent, such as those for esophageal cancer patients, while others are temporary and removed later.