Unit 3 - Diet and nutritional treatment approach for dysphagia
| Stránky: | IDEC TrainingCentre elearning |
| Kurz: | MODULE 1: METHODOLOGY AND TOOLS DEVELOPMENT FOR ADULT EDUCATORS |
| Kniha: | Unit 3 - Diet and nutritional treatment approach for dysphagia |
| Vytiskl(a): | Invitado |
| Datum: | Pátek, 6. února 2026, 23.26 |
Obsah
- 3.1. Basics of nutrition on dysphagia condition
- 3.1.1. Nutritional status and dysphagia
- 3.1.2. Nutritional requirements in patients with dysphagia
- 3.1.2.1. Correct energy balance.
- 3.1.2.2. Adequate macronutrient intake.
- 3.1.2.3. Dietary Reference Intake for vitamins and minerals
- 3.1.2.4. Optimal supply of bioactive compounds – phytochemicals
- 3.1.3. Relevance of the diagnosis of malnutrition in dysphagia
- 3.1.3.1. Malnutrition in patients with dysphagia
- 3.1.3.2. Identifying malnutrition in patients with dysphagia
- 3.1.3.3. Managing malnutrition in patients with dysphagia
- To know more
- 3.2. Balanced diet
- 3.2.4. Foods and ingredients for dysphagia diets
- 3.2.5. Balanced menu templates
- 3.2.6. Preparing meals
- 3.2.7. Additional products to use
3.1. Basics of nutrition on dysphagia condition
What will I learn in this lesson?
The aim of this lesson is to provide knowledge on nutrition in the dysphagia condition.
Learning outcomes
Understanding the importance of nutrition in the dysphagia condition.
Knowing the specific nutritional requirements in patients with dysphagia.
Identifying malnutrition in patients with dysphagia.
3.1.1. Nutritional status and dysphagia
Optimal nutritional status means providing all the nutrients in the right proportions to meet the individual's requirements to achieve the best performance and the longest possible lifetime in good health.
Improving nutritional status is a powerful factor in preventing and treating diseases and maintaining a good quality of life.
In view of the regular consumption of modified and/or less nutrient-dense meals, combined with difficulties in tolerating large volumes of fluids, dysphagic patients are at particularly high risk of inadequate macro- and micronutrient intakes.
Consequently, adults can suffer a negative energy balance, resulting in sustained weight loss, and their risk of sarcopenia, inadequate fluid intake and micronutrient deficiencies is increased. Referring to children, this situation can cause permanent, widespread damage to their growth, development and well-being.
The psychological implications of dysphagia should also be observed. Patients find increased dependence on caregiver at mealtimes and new feeding patterns, as degrading and upsetting, which may further lead to loss of appetite, depression and anxiety or fear at mealtimes – contributing to weight loss and exacerbation of malnutrition.
In fact, it is well-documented that dehydration and malnutrition, mainly undernutrition, are linked to undiagnosed or untreated dysphagia.
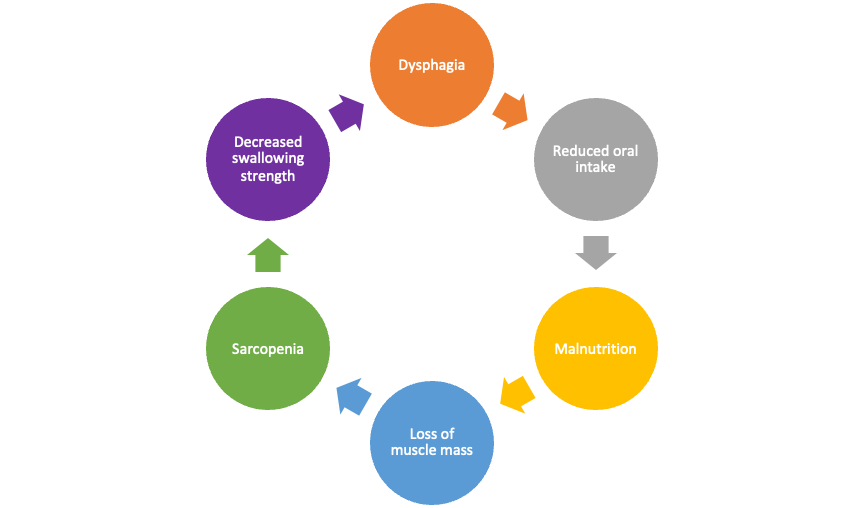
Malnutrition leads to systemic muscle mass loss and atrophy of the muscles used to swallow, and this ultimately leads to worsening of dysphagia.
Effective nutritional management is crucial to to maintain good nutritional status or to reverse malnutrition. The first step to stablish appropriate nutrition care plans is the nutrition assessment.
Goals of Nutritional Management:
Maintain and ensure adequate nutrition and hydration status;
Implement the correct and safe texture modified diet upon speech and language therapist recommendations;
Maximize nutritional intake while maintaining safe eating, i.e. to prevent aspiration and choking.
Establish the need for dietary supplementation and/or fortification.
3.1.2. Nutritional requirements in patients with dysphagia
3.1.2.1. Correct energy balance.
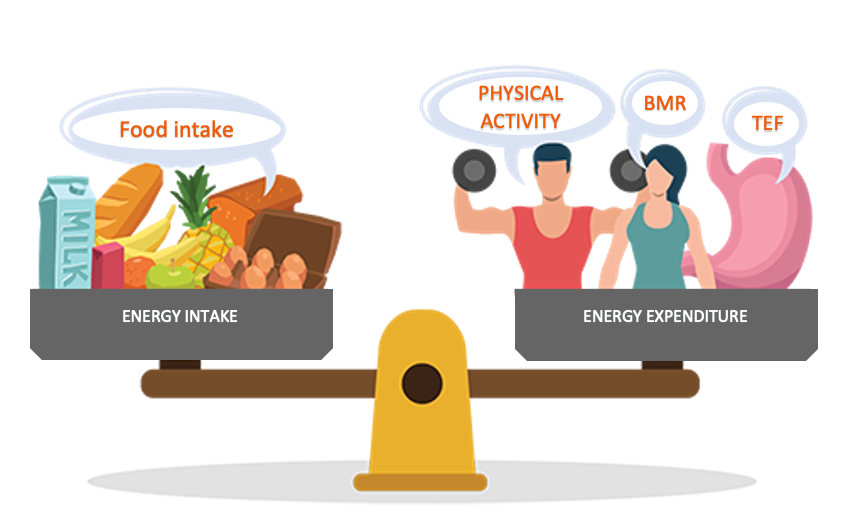
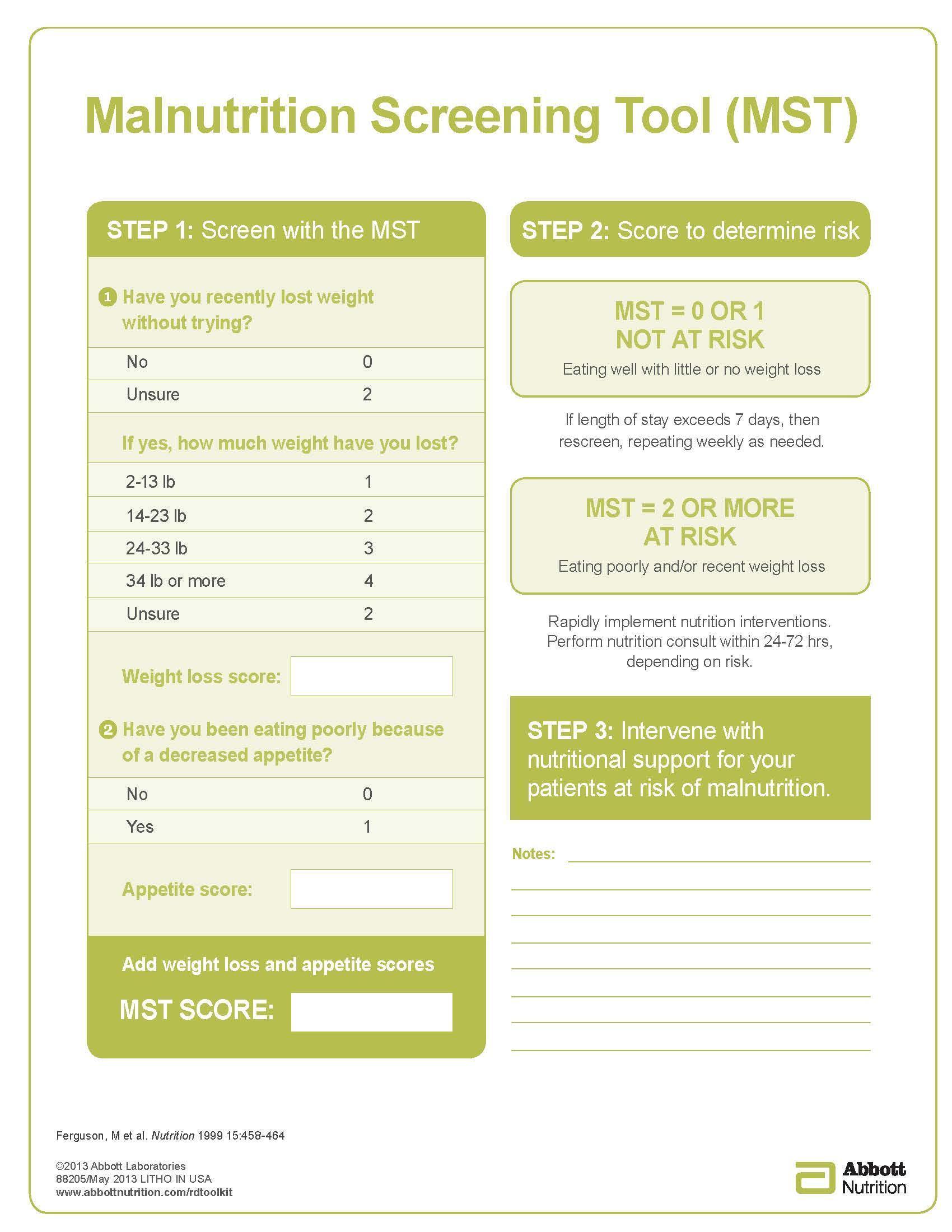
Figure 1. Components of the energy balance
Source: Modified image obtained from https://www.activehealth.sg/eat-better/resources/energy-balance
-
Energy intake: The number of calories in a food refers to the amount of energy stored in that food.
-
Energy expenditure: Your body uses calories:
-
Physical activity: walking, thinking, working, sports and so on.
-
Basal Metabolic Rate (BMR): vital physiological functions such as breathing, working of heart, etc.
-
Thermic Effect of Food (TEF): food digestion and absorption.
-
-
Correct energy balance:
-
Adults: The average adult person needs about 2,000 calories every day to maintain their weight, but the amount will depend on their age, sex, and physical activity level.

-
Children: The energy they need includes that used for their proper growth and development.
-
Specific situations: Some diseases require higher energy intake for better recovery.
-
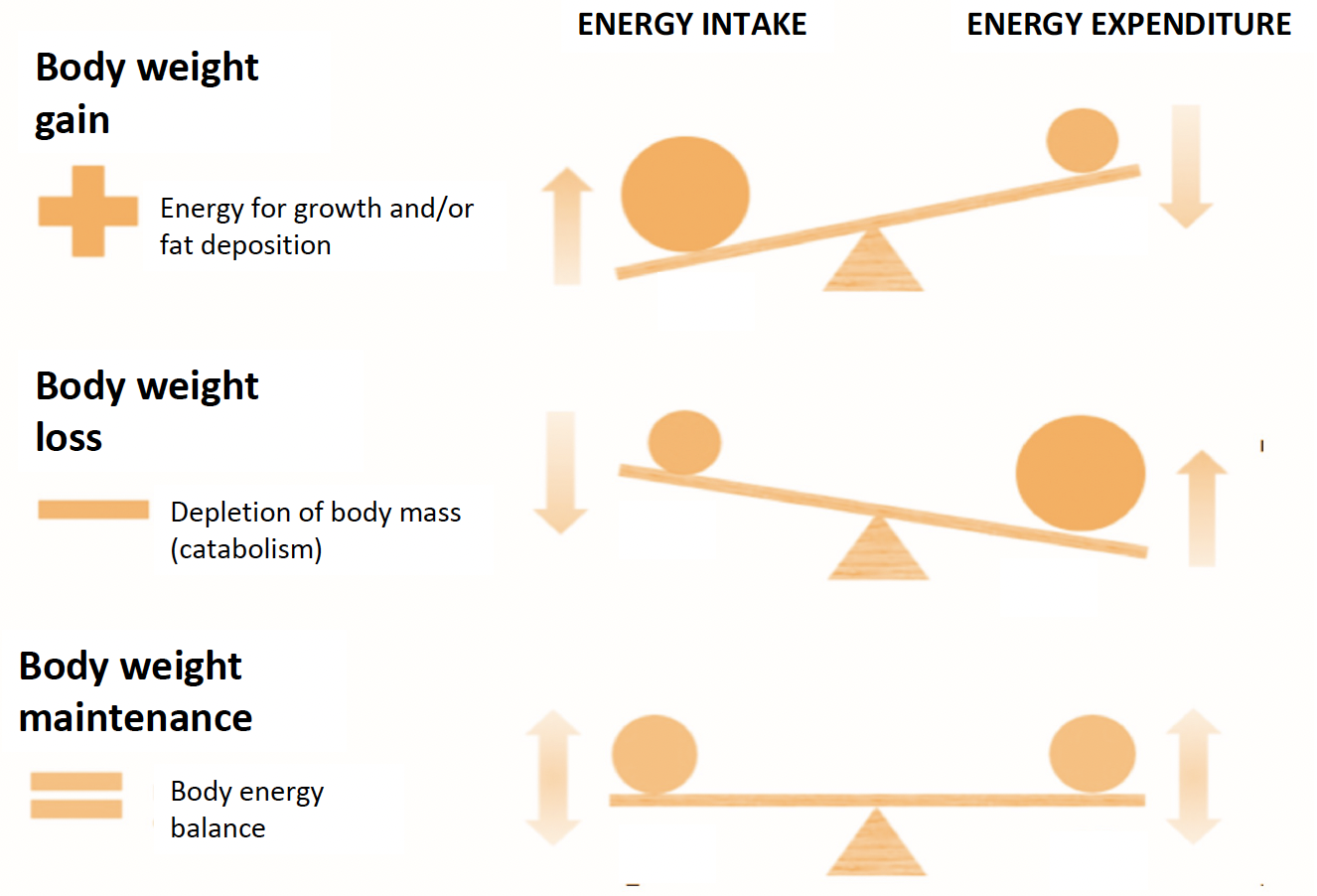
Figure 2. Different situations of energy balance
3.1.2.2. Adequate macronutrient intake.
Macronutrients:
Macronutrients are:
Proteins
Glycaemic carbohydrates
Dietary fibre
Fats
Water
They predominate in the composition of foodstuffs and, therefore, are daily ingested in quantities of grams.
Their main functions within the organism of proteins, fats and glycaemic carbohydrates are energetic and structural. Dietary fibre and water are considered regulatory nutrients.
Visit https://multimedia.efsa.europa.eu/drvs/index.htm to consult the Dietary Reference Values for the EU.
Proteins:
Dietary proteins are the source of nitrogen and essential aminoacids which the body requires for tissue growth and maintenance.

Main sources of protein could be plant and animal based.
Animal protein is a complete protein, containing all essential amino acids, and is considered a high biological value protein (HBV).
Plant proteins are incomplete proteins, providing only several essential amino acids to the diet, and are considered low biological value (LBV) proteins.
Protein complementation is when LBV proteins are combined: By eating two LBV proteins you can make up for the lacking amino acids in each, therefore giving an intake with a HBV i.e. legumes with cereals. There could also be protein complementation by eating adequate amounts of HBV and LBV proteins i.e. milk with bread.

Glycaemic carbohydrates:
They are the main source of energy, which they provide to body cells in the form of glucose.
Simple carbohydrates – Sugars: They are rapidly digested and absorbed in the human small intestine. Food containing sugars is prone to have a higher glycemic index. The amounts of dietary sugars should be low, and should preferably be sourced from nutritionally dense foods – i.e. fruits and fruit smoothies.

Complex carbohydrates – Starch: They are slower digested and absorbed in the human small intestine and a better choice as source of energy, mainly when these foods also contain dietary fibre. Main sources of carbohydrates and fibres should be form grits, porridges, mashed root and legumes.

Dietary fibre:
Carbohydrates which cannot be digested in the human small intestine and includes non-starch polysaccharides (cellulose, hemicellulose and pectins), resistant starch, resistant oligosaccharides, and lignin.
Dietary fibre has an established role in bowel function (e.g. laxation). Some types of dietary fibre also reduce absorption of dietary fat and glycaemic carbohydrates.
It is one of the most complicated nutrients, because naturally fibres present in nuts or grains can be difficult to consume by dysphagic patients. However, fruit and vegetables are also sources of dietary fibre.


![]()

Fat:
Fat is the most caloric-dense macronutrient.

Saturated and trans fat are usually solid at room temperature. Naturally-occurring in foodstuffs of animal origin, they are also very popular in (ultra-) processed foods. Butter, tallow, lard, coconut and palm oil are rich sources of saturated fat. Their intake, as well as that of cholesterol, should be limited.
![]()

- Unsaturated fat,
which are liquid at room temperature, are considered the “good“
fats because they play a high number of beneficial roles, mainly at
cardiovascular level.
- Monounsaturated fat should be the main type of fat to be ingested. Nuts, avocado, olive oil are sources of oleic acid, the most abundant monounsaturated fatty acid in foods.

![]()
Polyunsaturated fat. The most important polyunsaturated fatty acids are nutritionally essential, so it is compulsory in the diet:
Omega 3 fatty acids: alpha-linolenic acid (ALA), eicosapentaenoic acid and docosahexaenoic acid (EPA and DHA)
Omega 6 fatty acids: linoleic acid (LA)
Besides sources of energy, polyunsaturated fatty acids are considered regulators due to their role as precursors of important immunomodulatory compounds.



![]()
Did
you know ...?

In addition to those present as components of foodstuffs, fats can be served as sauces or consumed by adding in smashed food, not only to increase energy intake, but also improve the taste.
Source: https://www.pexels.com/

Source: https://pixbay.com/
Water:
Almost every cell in human body contains water: body water makes up 79% of muscles, 73% of brain, and even 31% of bones. Overall body weight can be 45-65% water.

Source: designed by Canva Pro
Water is essential for practically all functions of the body. It helps to restore fluids lost through metabolism, breathing, sweating, and the removal of waste. Besides, it is particularly important for thermoregulation. Finally, it lubricates the joints and tissues, maintains healthy skin, and is necessary for proper digestion.
Source: designed by Canva Pro

A human can go without food for about three weeks but would typically only last three to four days without water.
Source: https://pixabay.com/
Keep in mind that about 20% of our total water intake comes not from beverages but from water-rich foods such as fruits and vegetables.
Source: https://pixabay.com/

ACTIVITY ABOUT MACRONUTRIENTS:
3.1.2.3. Dietary Reference Intake for vitamins and minerals
Micronutrients-
Micronutrients are:
-
Vitamins:
- Water-soluble vitamins
- Fat-soluble vitamins
-
Vitamins:
-
Minerals
- Macrominerals
- Microminerals or trace elements
- Micronutrients are non-energetic nutrients but they are essential for healthy development, disease prevention, and wellbeing due to their functions as, mainly, regulatory compounds.
- The organism needs micronutrients in small quantities (milligrams or, even, micrograms), but it is essential to provide them in the diet because the human organism is not able to synthesise them (or only in insufficient quantities).
- There is no single food that contains all the essential vitamins and minerals for human beings.
- Visit https://multimedia.efsa.europa.eu/drvs/index.htm to consult the Dietary Reference Values for the EU.
Vitamins:
-
13 organic substances, with lots of different regulatory functions, are
considered vitamins. Vitamins play a vital role in many biochemical
functions in the human body and are essential components for
maintaining optimal health.
-
Water-soluble vitamins: They are characterised by their ability to dissolve in
water. Therefore, in general, their absorption in the small
intestine is easier, their storage in the body is very limited and unused amounts and/or their metabolites are eliminated in the
urine.
There are 9 water-soluble vitamins: the B-complex vitamins, thiamine, riboflavin, niacin, pantothenic acid, biotin, vitamin B6, folate, and vitamin B12, and vitamin C.
-
Fat-soluble vitamins: There are 4 fat-soluble vitamins: vitamins A - retinol,
D - cholecalciferol, E - tocopherol, and K.
They dissolve in fat. Due to their low solubility in hydrophilic media, the body absorbs them into newly forming micelles in the small intestine. Besides, they need specific ways of transport in the body and tend to accumulate in the tissues.
Retinol is present in animal-based food, but carotenoids from plant-based food can be converted by the body into retinol.
Cholecalciferol can be synthesised in the skin by the action of ultraviolet rays.
Vitamin K synthesised by intestinal bacteria can be used by the organism.
-
Water-soluble vitamins: They are characterised by their ability to dissolve in
water. Therefore, in general, their absorption in the small
intestine is easier, their storage in the body is very limited and unused amounts and/or their metabolites are eliminated in the
urine.
Minerals:
-
They are inorganic substances that are responsible for structural functions
involving the skeleton and soft tissues and for regulatory
functions including neuromuscular transmission, blood clotting,
oxygen transport, and enzymatic activity.
- Macrominerals: Calcium, magnesium, phosphorus and the electrolytes, sodium, potassium and chloride, are considered essential macrominerals
- Microminerals or trace elements: Iron, zinc, copper, iodine, selenium are considered essential the most important trace elements.
Did you know ...?
- Eating a wide variety of foods is the best way to get the necessary amounts of vitamins and minerals.
- Some micronutrients are present in a small number of foods i.e. foods from animals, but not plants, naturally have vitamin B12.
Source: https://www.clinicabaviera.com/
ACTIVITY ABOUT MICRONUTRIENTS:
3.1.2.4. Optimal supply of bioactive compounds – phytochemicals
-
They are interesting naturally occurring compounds, mainly in plant-based food (that is why they are known as phytochemicals), that are not considered nutrients.

Figure 3. Major
food bioactive compounds sources
Obtained from: Câmara JS, Albuquerque BR, Aguiar J, Corrêa RCG, Gonçalves JL, Granato D, et al. Food Bioactive Compounds and Emerging Techniques for Their Extraction: Polyphenols as a Case Study. Foods 2021, 10, 37. https://doi.org/10.3390/foods10010037
-
Bioactive compounds are thought to be largely responsible for the protective health benefits of these plant-based foods and beverages, beyond those conferred by their nutritional value.
-
These phytochemicals, which are part of a large and varied group of chemical compounds, also are responsible for the color, flavor, and odor of plant foods, such as blueberries’ dark hue, broccoli’s bitter taste, and garlic’s pungent odor.
-
Research strongly suggests that consuming foods rich in phytochemicals provides health benefits, but not enough information exists to make specific recommendations for phytochemical intake.

3.1.3. Relevance of the diagnosis of malnutrition in dysphagia
3.1.3.1. Malnutrition in patients with dysphagia
Malnutrition refers to deficiencies, excesses, or imbalances in a person’s intake of energy and/or nutrients:
Undernutrition, which includes wasting (low weight-for-height), stunting (low height-for-age) and underweight (low weight-for-age);
Micronutrient-related malnutrition, which includes micronutrient deficiencies (a lack of important vitamins and minerals) or micronutrient excess; and
Overweight and obesity.
It is known that various pathological conditions may cause malnutrition, but many, even healthy, dysphagic people may fail to adequately consume food and experience any type of malnutrition.
Dysphagia and malnutrition are apparently associated. Several studies have focused on dysphagia as a prevalent risk factor for malnutrition during recent years.
Untreated dysphagia patients who are malnourished sustain a longer hospital stay, higher risk of complications, and higher mortality rate than those who are properly nourished.
Did you know ...?
The prevalence of concurrent malnutrition and dysphagia has been estimated between 3% and 29% in the elderly. Vitamin B12, C, D, folate, zinc and iron are the micronutrients to pay most attention to.
The prevalence of oropharyngeal dysphagia in children with cerebral palsy is estimated to be between 19% and 99%. A recent review found a high rate of malnutrition in children with cerebral palsy and several nutrient deficiencies were detected such as hypocalcemia and reduced serum concentrations of zinc, copper, and vitamin D.
The presence of dysphagia is a major risk factor for developing malnutrition in stroke patients.
It is difficult to accurately ascertain the prevalence of malnutrition in dysphagic people due to discrepancies in the measurement methods used.
Reduced oral intake due to dysphagia leads to weight loss and disrupted synthesis of skeletal muscles, which consequently result in further development of sarcopenia. Therefore, a vicious cycle between dysphagia, malnutrition, and sarcopenia eventually becomes inevitable.
3.1.3.2. Identifying malnutrition in patients with dysphagia
 Early referral to the clinical
nutritionist has a pivotal importance in halting the progressive
nature of malnutrition and allowing close monitoring of patients’
weight and oral intake and the tolerability of the prescribed diet.
Early referral to the clinical
nutritionist has a pivotal importance in halting the progressive
nature of malnutrition and allowing close monitoring of patients’
weight and oral intake and the tolerability of the prescribed diet.
Health professionals must do nutrition screening to detect patients at risk of malnutrition.
The clinical nutritionist carries out a full nutritional status assessment and the results determine the dietary counselling and/or treatment.
Source: obtained from Canva Pro
-
Nutritional status screening:
Nutritional status screening ...
-
is a process to identify an individual who is malnourished or at risk of being malnourished.
-
is used to determine whether a full nutrition assessment is indicated.
-
is generally completed by someone other than the nutrition provider.
Malnutrition risk screening (MNRS) tools …
-
should be quick, simple, and easy to use
-
a certain degree of validity, agreement, and inter-rater reability in identifying malnutrition risk is necessary
-
MNRS for adults:

-
MST – Malnutrition Screening Tool
-
MUST – Malnutrition Universal Screening Tool

-
MNRS for elderly:

-
MNA – Mini Nutritional Assessment

Source: https://pixabay.com/


-
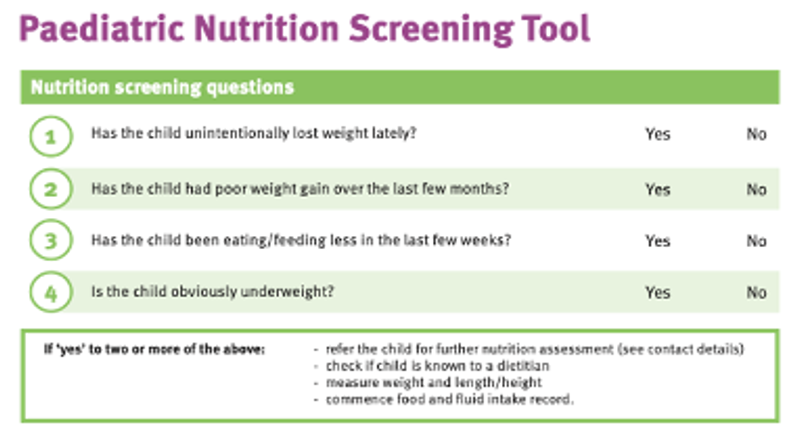
Paediatric MNRS:
-
STAMP – Screening Tool for Assessment of Malnutrition in Paediatrics.
-
PNST – Paediatric Nutrition Screening Tool.
Source: https://www.pngegg.com/

Nutritional status assessment:
Nutritional status assessment ...
-
is used to determine the nutritional status of individual or population groups as influenced by the intake and utilization of nutrients
-
can be defined as the interpretation from dietary, laboratory, anthropometric, and clinical studies.
An easy way to remember the components of the nutritional status assessment is:
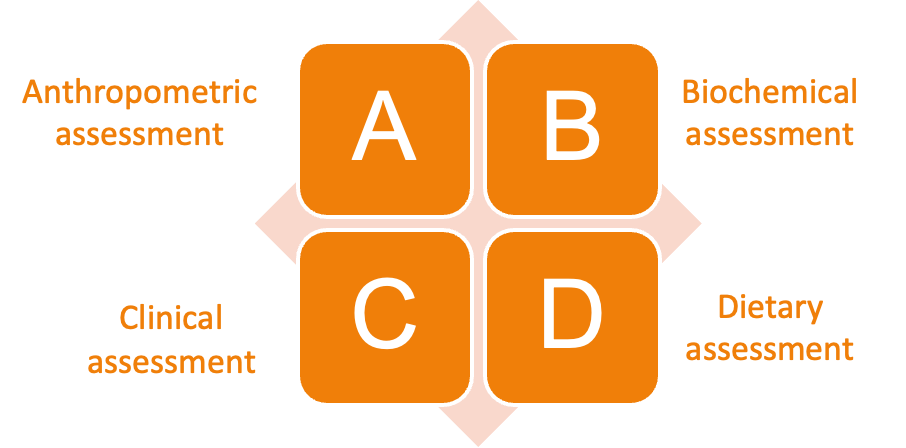


-
ANTHROPOMETRIC ASSESSMENT:
Consists in the measurement of the size, weight and proportions of the body.
Source: https://medicaltrain.es/
The most common measurements are weight,
height, perimeters and skin folds.
-
BIOCHEMICAL ASSESSMENT:
Uses laboratory
measurements of serum protein, serum micronutrient levels, serum
lipids, and immunological parameters to assess general nutritional
status and to identify specific nutritional deficiencies. Urine and
stools samples may also be analysed.
Source: https://pixabay.com/
-
CLINICAL ASSESSMENT:
The estimation of
nutritional status on the basis of recording a medical history and
conducting a physical examination to detect signs (observations made
by a qualified observer) and symptoms (manifestations reported by the
patient) associated with malnutrition. Some sociodemographic and
psychological factors related to nutritional status are also
collected.
Source: https://pixabay.com/
-
DIETARY ASSESSMENT:
It provides information on dietary
quantity and quality and the results are compared with recommended
intake.
Several common methods to assess dietary intake exist: 24h-recall, food-frequency questionnaires and food weighted records
Source: https://pixabay.com/
3.1.3.3. Managing malnutrition in patients with dysphagia
In order to overcome the problem of malnutrition, a team approach including medical doctors, dentists, nurses, public health nurses, nutritionists, and therapists is mandatory.
Actions:
-
Remove or substantially modify dietary restrictions;
-
Encourage use of flavor enhancers and frequent small meals;
-
Improve protein and energy intake by enrichment meals;
-
Treat depression, and remove or replace medicines that can cause loss of appetite as a side-effect,
-
Offer liquid nutritional supplements for use between (not with) meals;
-
Evaluate swallowing as well as functional ability to manage eating;
-
If the patient must be fed, allow adequate time for chewing, swallowing, and clearing throat before offering another bite.
To know more
Ueshima J, et al. Nutritional Assessment in Adult Patients with Dysphagia: A Scoping Review. Nutrients. 2021 Feb 27;13(3):778. doi: 10.3390/nu13030778.
Rodd BG, et al. Dysphagia, texture modification, the elderly and micronutrient deficiency: a review. Crit Rev Food Sci Nutr. 2021 Apr 27:1-17. doi: 10.1080/10408398.2021.1913571.
da Silva DCG, et al. Malnutrition and nutritional deficiencies in children with cerebral palsy: a systematic review and meta-analysis. Public Health. 2022 Apr;205:192-201. doi: 10.1016/j.puhe.2022.01.024.
Huppertz V, et al. Impaired Nutritional Condition After Stroke From the Hyperacute to the Chronic Phase: A Systematic Review and Meta-Analysis. Front Neurol. 2022 Feb 1;12:780080. doi: 10.3389/fneur.2021.780080.
Chen KC, Jeng Y, Wu WT, Wang TG, Han DS, Özçakar L, Chang KV. Sarcopenic Dysphagia: A Narrative Review from Diagnosis to Intervention. Nutrients. 2021 Nov 12;13(11):4043. doi: 10.3390/nu13114043.
Skipper A, Coltman A, Tomesko J, Charney P, Porcari J, Piemonte TA, Handu D, Cheng FW. Adult Malnutrition (Undernutrition) Screening: An Evidence Analysis Center Systematic Review. J Acad Nutr Diet. 2020 Apr;120(4):669-708. doi: 10.1016/j.jand.2019.09.010.
Skipper A, Coltman A, Tomesko J, Charney P, Porcari J, Piemonte TA, Handu D, Cheng FW. Position of the Academy of Nutrition and Dietetics: Malnutrition (Undernutrition) Screening Tools for All Adults. J Acad Nutr Diet. 2020 Apr;120(4):709-713. doi: 10.1016/j.jand.2019.09.011.
Isautier JMJ, Bosnić M, Yeung SSY, Trappenburg MC, Meskers CGM, Whittaker AC, Maier AB. Validity of Nutritional Screening Tools for Community-Dwelling Older Adults: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc. 2019 Oct;20(10):1351.e13-1351.e25. doi: 10.1016/j.jamda.2019.06. 024.
Wu XS, Miles A, Braakhuis AJ. Texture-Modified Diets, Nutritional Status and Mealtime Satisfaction: A Systematic Review. Healthcare (Basel). 2021 May 24;9(6):624. doi: 10.3390/healthcare9060624.
Becker PJ, Gunnell Bellini S, Wong Vega M, Corkins MR, Spear BA, Spoede E, Hoy MK, Piemonte TA, Rozga M. Validity and Reliability of Pediatric Nutrition Screening Tools for Hospital, Outpatient, and Community Settings: A 2018 Evidence Analysis Center Systematic Review. J Acad Nutr Diet. 2020 Feb;120(2):288-318.e2. doi: 10.1016/j.jand.2019.06.257.
Becker PJ, Brunet-Wood MK. Pediatric malnutrition screening and assessment tools: Analyzing the gaps. Nutr Clin Pract. 2022 Oct;37(5):1088-1104. doi: 10.1002/ncp.10793.
3.2. Balanced diet
What will I learn in this lesson?
The aim of this lesson is to provide the necessary knowledge to develop a balanced diet to ensure an adequate nutritional status of people suffering from dysphagia.
Learning outcomes
To develop understanding of distribution of foodstuffs on a balanced diet in order to ensure dietary adequacy;
To recognize the benefits of nutrition fortification and using supplements;
To apply knowledge and create a menu template.
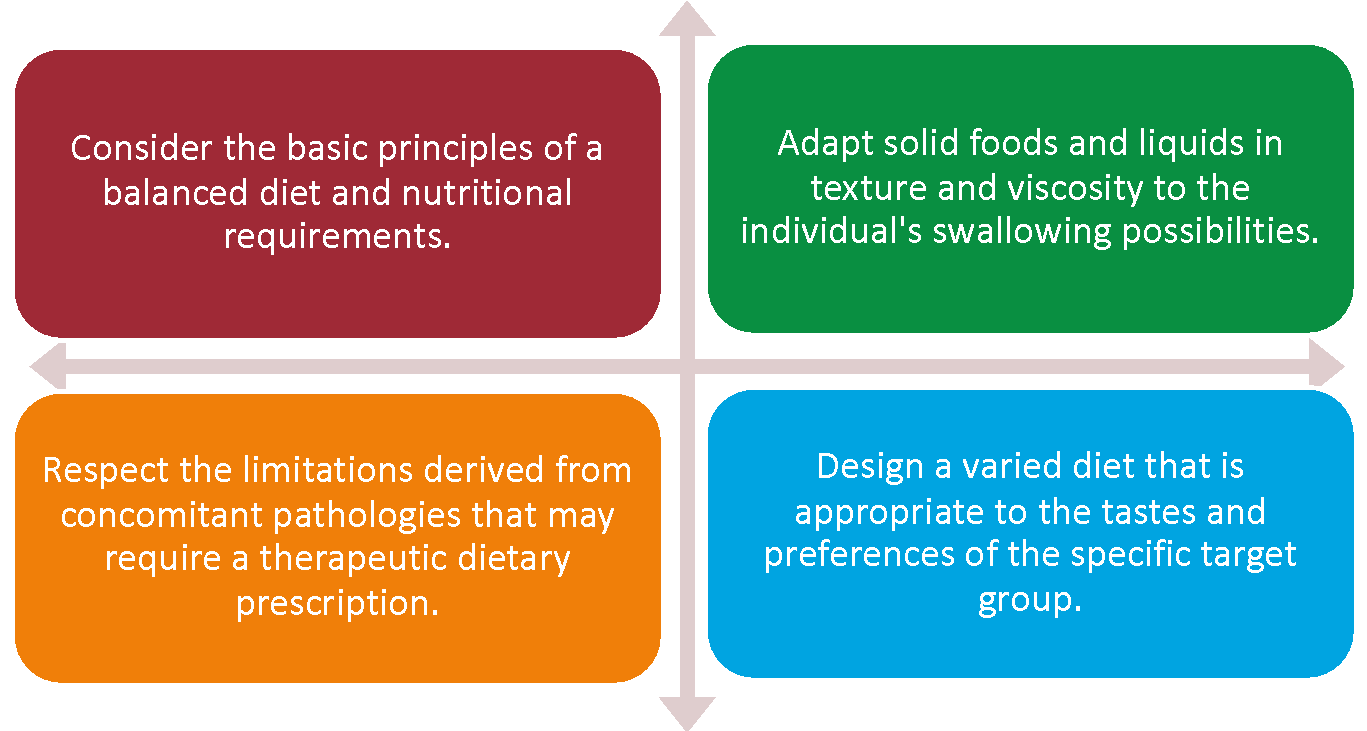
3.2.1. Criteria of the dysphagia diet
Focus on...
-
To ensure an adequate supply of energy, macro and micronutrients, it is essential to take into account the characteristics of the dysphagic individual.
-
Short-term or long-term dysphagia. If dysphagia is temporary – many patients will be able to progress to a wider variety of foods and more normal textures, as swallowing functions improves. If dysphagia is certain neurological and degenerative disease, deterioration is progressive and inevitable.
-
Meal fortification. Liquid added to food should have some nutritional value. Higher caloric additions, such as full fat milk, cream, butter and sauces, provide extra energy and several nutrients.
-
Diet supplementation
3.2.2. Distribution of foodstuffs on a balanced diet
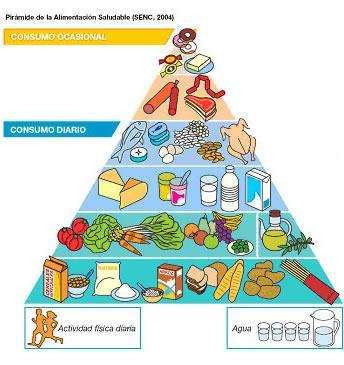
A balanced diet gives the body the nutrients it needs to function correctly. In order to get the nutrients needed, most of the daily caloric intake in should come from:
-
fresh fruits & vegetables;
-
whole grains;
-
protein rich foods (legumes; meat; fish)
-
dairy products;
-
fats and oils
In practice, a balanced diet means that we should eat a variety of foods, in different proportions, and in general avoid leaving out entire food groups, as each food group provides fuel and nutrients required for optimal health.
Food-Based Dietary Guidelines (FBDG) are developed to help people build a balanced and varied diet by following the food groups and consuming them in the right proportions.
-
Food-Based Dietary Guidelines (FBDG) in Europe
FBDG advice on foods, food groups and dietary patterns to provide the required nutrients to the general public to promote overall health and prevent chronic diseases
Some
countries provide a graphic representation, such as a food pyramid or
a plate, to illustrate and sum-up the advice.

Watch
this video to learn what are and how to use Dietary Guidelines:

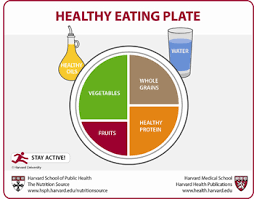
The Harvard Eating Plate is more widely accepted nowadays than the Food Pyramid. Find out more
here: https://www.hsph.harvard.edu/nutritionsource/healthy-eating-plate/
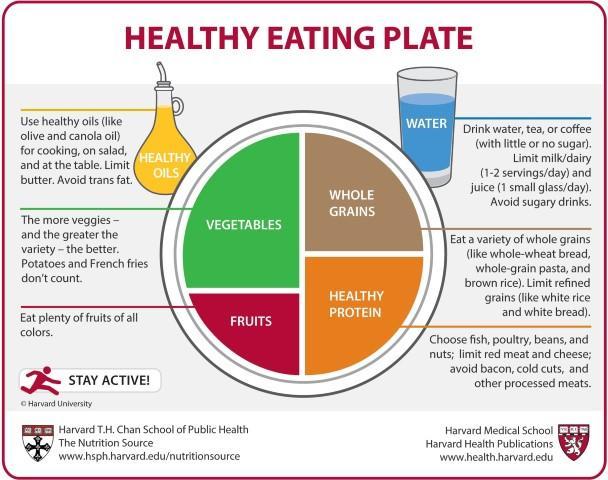
-
A balanced diet consists on:
-
Fruits & Vegetables should make up the largest portion of our diet. They contain a wide variety of nutrients like several vitamins and minerals, carbohydrates and dietary fibre. They are also the main source of phytochemicals.

Source: designed by Canva Pro
-
It is recommended to choose mostly whole grains (such as brown rice, oats and barley), and whole meal/wholegrain/high cereal/fibre varieties of bread, pasta, crispbreads and cereal foods. They mainly provide starch and fiber, but they are sources of several important vitamins and minerals.
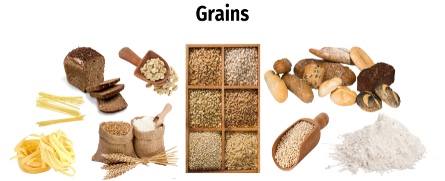
Source: designed by Canva Pro
-
Varied protein rich foods
 Dairy
products as milk, natural yoghurt or cheese, primarily provide us
with calcium, protein and fats, plus other vitamins and minerals.
Dairy
products as milk, natural yoghurt or cheese, primarily provide us
with calcium, protein and fats, plus other vitamins and minerals.
Red meat is high in saturated fat, vitamin B12, iron, niacin, and zinc. Meanwhile, fish is a great source of omega-3 fatty acids, vitamin D, thiamine, selenium, and iodine.
Vitamin A, B12, iron, and selenium are present in significant amounts in liver and other organ meats. These meats are also excellent sources of choline, an important nutrient for brain, muscle, and liver health.
Meat is a rich source of protein and several vitamins and minerals, including vitamin B12, niacin, and selenium.
Source: obtained from Canva Pro
-
Use healthy fats.
Olive oil, canola oil and seed oils are useful for cooking and are sources of heart-healthymonounsaturated and polyunsaturated fats. Tree nuts and fish are also sources of healthypolyunsaturated fats, including omega-3s.

Source: obtained from Canva Pro
-
Choose water as your main drink, and avoid sugary options such as soft drinks, sports drinks and energy drinks.
Drink fluids, even you don’t feel thirst!
Source: obtained from Canva Pro
-
Seasoning. Herbs and spices provide a wonderful range of flavours and aromas to our food. Limit added salt and sugar.


Source: obtained from Canva Pro Source: designed by Canva Pro
-
Mediterranean Diet: healthy and sustainable dietary pattern
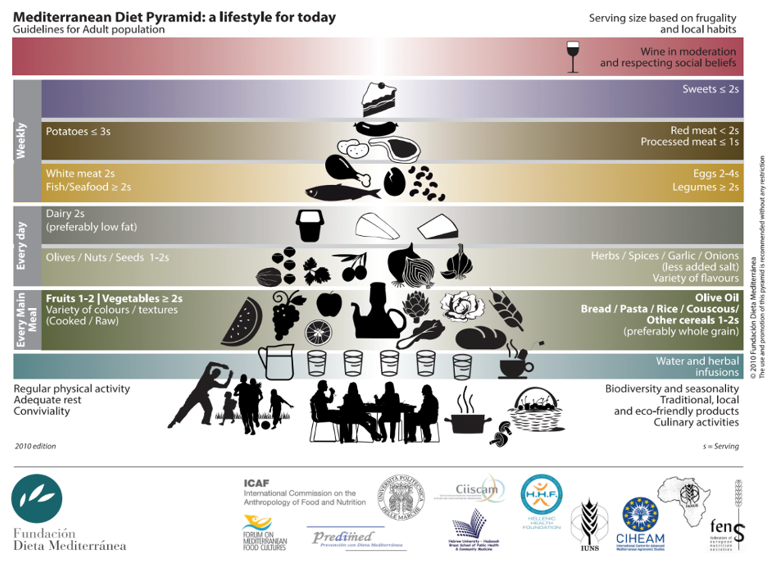
Find out more about Mediterranean Diet here: https://dietamediterranea.com/

3.2.3. Ensuring dietary adequacy
Guides of portion sizes

There really is no 'One Size Fits All‘ diet
Visit this site for more information about portion sizes: https://www.eufic.org/en/healthy-living/category/portion-information

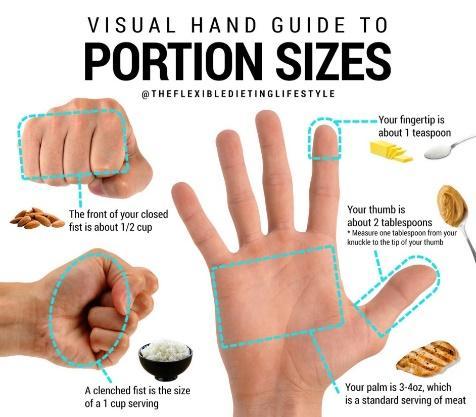
Source: Signature Nutrition Clinic Source: @Zach_Rochelaeu
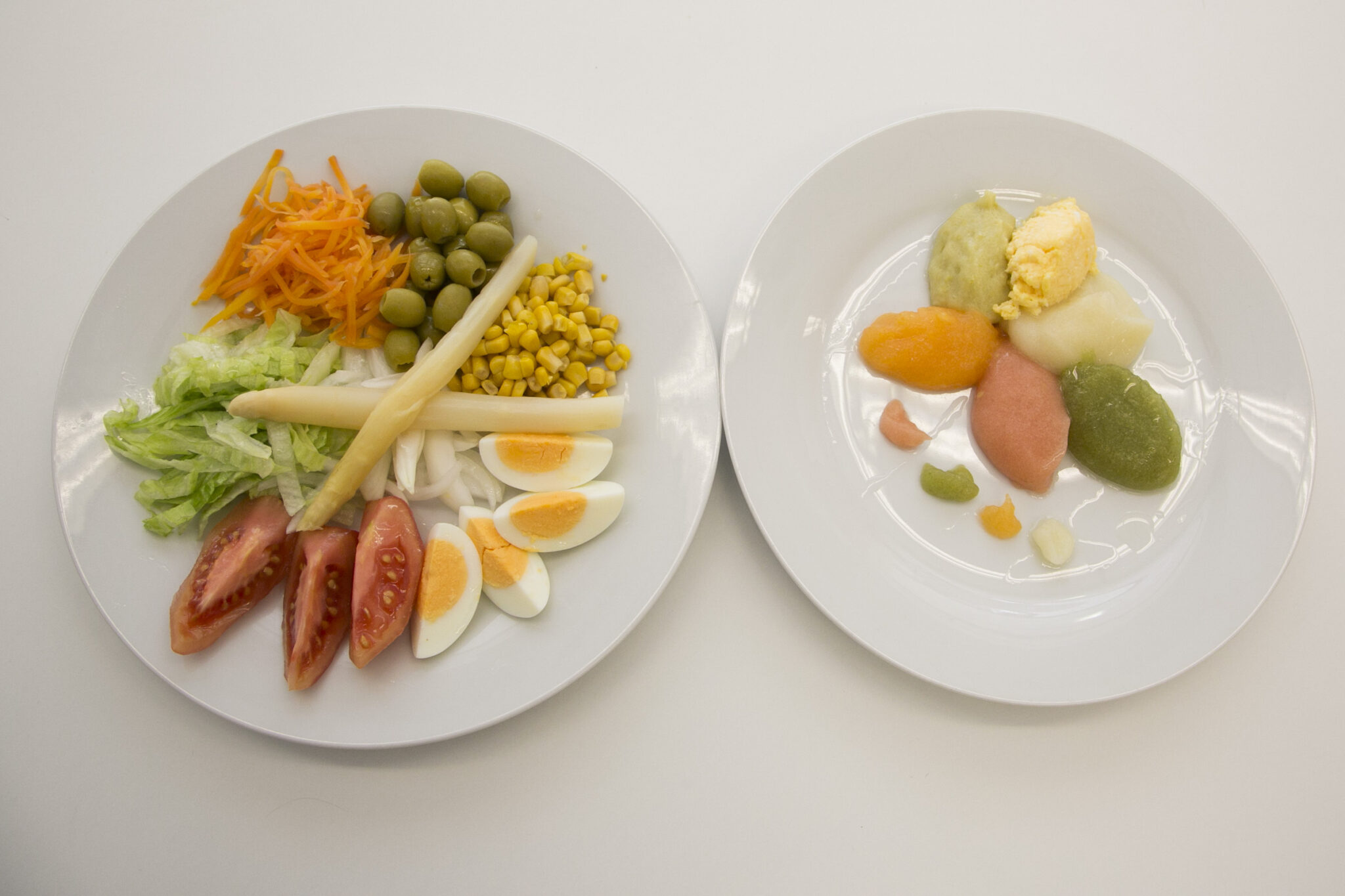
A modified consistency diet should be:

Nutritionally adequate;
Of correct consistency;
Appetising and palatable;
Well presented – considering color coordination and garnishes
Source: https://orpea.es/comida-texturizada-solucion-para-los-problemas-de-alimentacion-en-personas-mayores/
The Dietary Guidelines are different in each European country. However, there is some basic knowledge about dysphagia diet that should be taken into consideration when acquiring knowledge about this condition:
Consulting with a speech-language pathologist, dietitian, or healthcare professional trained in treating swallowing disorders can be critical for finding foods that are safe and nutritious while also aesthetically pleasing and appetizing. They can help you design the most permissive yet safe modified dysphagia diet of soft, minced or moist, puréed, or liquefied food.
Providing patients with meals that look and taste natural can increase consumption and prevent malnutrition.
For those consuming regular easy-to-chew foods, instill a sense of independence by providing patients with adaptive eating tools like plates with large rims, cups with lids and wide bases, and non-slip placemats. If a patient has difficulty using cutlery, serve bite-sized finger foods that are easy to pick up, such as chicken nuggets, fish sticks, cheese sticks, orange segments, carrot sticks, or steamed broccoli.
Serve food when patients are most alert and attentive. Some might eat better if they are provided with smaller dishes throughout the day, which can be less daunting than three large meals.
Make mealtime more pleasurable by engaging all of a patient’s senses during food preparation. Before cooking, bring ingredients, such as vegetables and fruits, to the patient so they can see and smell them, and use seasonal ingredients to make iconic dishes of summer, fall, winter, and spring.
3.2.4. Foods and ingredients for dysphagia diets
3.2.4.1. Recommended and inappropriate foods and ingredients
The following are some of the permitted foods:
Pureed breads (also called “pre-gelled” breads)
Smooth puddings, custards, yogurts, and pureed desserts
Pureed fruits and well-mashed bananas
Pureed meats
Souffles
Well-moistened mashed potatoes
Pureed soups
Pureed vegetables without lumps, chunks, or seeds
It is important to avoid other foods, including:
Non-pureed breads
Any cereal with lumps
Cookies, cakes, or pastry
Whole fruit
Non-pureed meats, beans, or cheese
Scrambled, fried, or hard-boiled eggs
Non-pureed potatoes, pasta, or rice
Non-pureed soups
Non-pureed vegetables
Seeds, nuts, or chewy candies
In each of the groups you should choose …
Vegetables and fruits:
Soft diced cooked vegetables (carrots, squash), mashable cooked vegetables (peas, spinach)
Minced cooked vegetables (broccoli, yellow or green beans)
Very finely shredded or minced salads (coleslaw, leafy greens, lettuce) with extra dressing if needed.
Mashed potatoes or other well-cooked potato side dishes such as scalloped potatoes.
Canned cream corn.
Soft ripe mashable fruit: canned, fresh, or frozen(bananas, canned crushed pineapple, canned mandarin oranges, canned sliced peaches, ripe pears), fresh fruit with skins and membranes removed (diced soft cantaloupe, seedless watermelon) fruit cocktail without pineapple pieces or grapes.
Pureed, stewed pitted prunes.
Fruit smoothies.
Grain foods:
Cooked cereals (cream of rice, cream of wheat®oat bran, oatmeal).
Cold cereals that soften in milk (bran flakes, corn flakes, rice crisps).
Soft moist bread products (biscuits, buns, buttered toast, muffins) served with butter, soft margarine, or other allowed spreads.
French toast, pancakes, or waffles, served with applesauce or syrup to moisten
Soft moist barley, couscous, quinoa, or rice in sauces, soups, or casseroles.
Pasta served in sauce.
Bread pudding, or soft and moist bread stuffing (without chocolate chips, coconut, dried fruit, nuts, seeds, or any other hard particles).
Soft crackers, such as soda crackers.
Soft cereal bars, such as nutri-grain® bars.
Ground flax seed or wheat bran stirred into cereals.
Protein foods:
Milk: plain or flavoured.
Buttermilk, smooth milkshakes, or fortified soy beverages.
Smooth yogurt or fruit yogurt with small soft pieces of fruit.
Cottage cheese, all cheeses (hard or soft), diced, sliced, or grated.
Soft tofu/soy protein.
Soft cooked beans, lentils, peas, or soft dishes made with allowed ingredients (soft bean salad).
Smooth nut butters mixed into allowed foods (peanut butter smoothie).
All cooked eggs or egg substitutes including omelets and quiche, made with allowed foods.
Soft moist tender meat or poultry, diced.
Canned fish with bones removed (canned salmon with mashed bones is allowed).
Tender boneless fish that flakes easily.
Thinly shaved soft deli meats (roast beef, turkey, ham).
Sandwiches with finely-minced salad-type fillings (egg, chicken, tuna salad, minced lettuce, or cheese) without whole lettuce or whole raw vegetables.
Tender mashable meats, made with allowed ingredients (casseroles, lasagna, meatloaf, meatballs).
Soft and mashable perogies, served with allowed condiments.
Stir-fry made with allowed ingredients.
Spaghetti sauces made with allowed ingredients.
Broth or cream soups made with allowed ingredients.
Desserts and snacks:
Ice cream, popsicles®, sherbet, soy frozen desserts, or frozen yogurt.
Smooth custards, milk pudding, mousse, rice pudding, or tapioca pudding.
Soft, moist, or easy-to-break cookies (digestive biscuits).
Soft baked desserts (cream or pumpkin pies, moist cakes) made with allowed foods.
Jellied desserts.
Condiments and sauces:
Butter, soft margarine, mayonnaise, salad dressings, or sour cream.
Condiments that are smooth, or have small pieces such as BBQ sauce, horseradish, ketchup, mustard, or relish.
Finely ground herbs, seasonings, and spices, without hard seeds.
Gravies or sauces that are smooth such as cheese sauce, hollandaise sauce, orwhite sauce.
Soft, mashable jam and jelly, without seeds or hard pieces.
Sugar, syrup, or sugar substitutes.
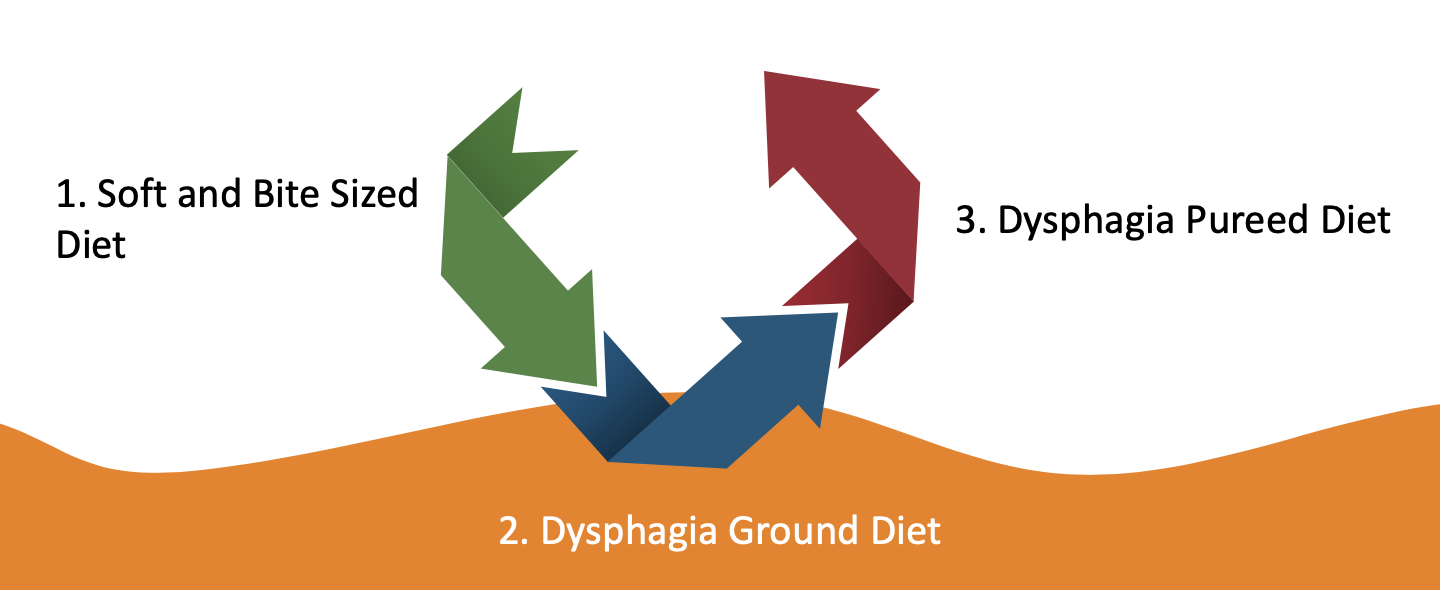
3.2.4.2. Dysphagia diet may be adapted to three levels
-
Food products: Protein foods
|
1. Dysphagia Soft and Bite Sized Diet |
2. Dysphagia Ground Diet |
3. Dysphagia Pureed Diet |
|
|
|
To avoid
|
1. Dysphagia Soft and Bite Sized Diet |
2. Dysphagia Ground Diet |
3. Dysphagia Pureed Diet |
|
|
|
-
Food products: milk, yoghourt, cheese
|
1. Dysphagia Soft and Bite Sized Diet |
2. Dysphagia Ground Diet |
3. Dysphagia Pureed Diet |
|
|
|
To avoid
|
1. Dysphagia Soft and Bite Sized Diet |
2. Dysphagia Ground Diet |
3. Dysphagia Pureed Diet |
|
|
|
-
Food products: soups
|
1. Dysphagia Soft and Bite Sized Diet |
2. Dysphagia Ground Diet |
3. Dysphagia Pureed Diet |
|
|
|
To avoid
|
1. Dysphagia Soft and Bite Sized Diet |
2. Dysphagia Ground Diet |
3. Dysphagia Pureed Diet |
|
|
|
-
Food products: grains, cereals, breads, starches
|
1. Dysphagia Soft and Bite Sized Diet |
2. Dysphagia Ground Diet |
3. Dysphagia Pureed Diet |
|
|
|
To avoid
|
1. Dysphagia Soft and Bite Sized Diet |
2. Dysphagia Ground Diet |
3. Dysphagia Pureed Diet |
|
|
|
-
Food products: fruits and vegetables
|
1. Dysphagia Soft and Bite Sized Diet |
2. Dysphagia Ground Diet |
3. Dysphagia Pureed Diet |
|
|
|
To avoid
|
1. Dysphagia Soft and Bite Sized Diet |
2. Dysphagia Ground Diet |
3. Dysphagia Pureed Diet |
|
|
|
-
Food products: condiments
|
1. Dysphagia Soft and Bite Sized Diet |
2. Dysphagia Ground Diet |
3. Dysphagia Pureed Diet |
|
|
|
To avoid
|
1. Dysphagia Soft and Bite Sized Diet |
2. Dysphagia Ground Diet |
3. Dysphagia Pureed Diet |
|
|
|
-
Food products: desserts
|
1. Dysphagia Soft and Bite Sized Diet |
2. Dysphagia Ground Diet |
3. Dysphagia Pureed Diet |
|
|
|
To avoid
|
1. Dysphagia Soft and Bite Sized Diet |
2. Dysphagia Ground Diet |
3. Dysphagia Pureed Diet |
|
|
|
-
Food products: beverages
You can choose any smooth, homogenous beverages without lumps, chunks, or pulp. Beverages may need to be thickened to appropriate consistency
You must avoid any beverages with lumps, chunks, seeds, pulp, etc

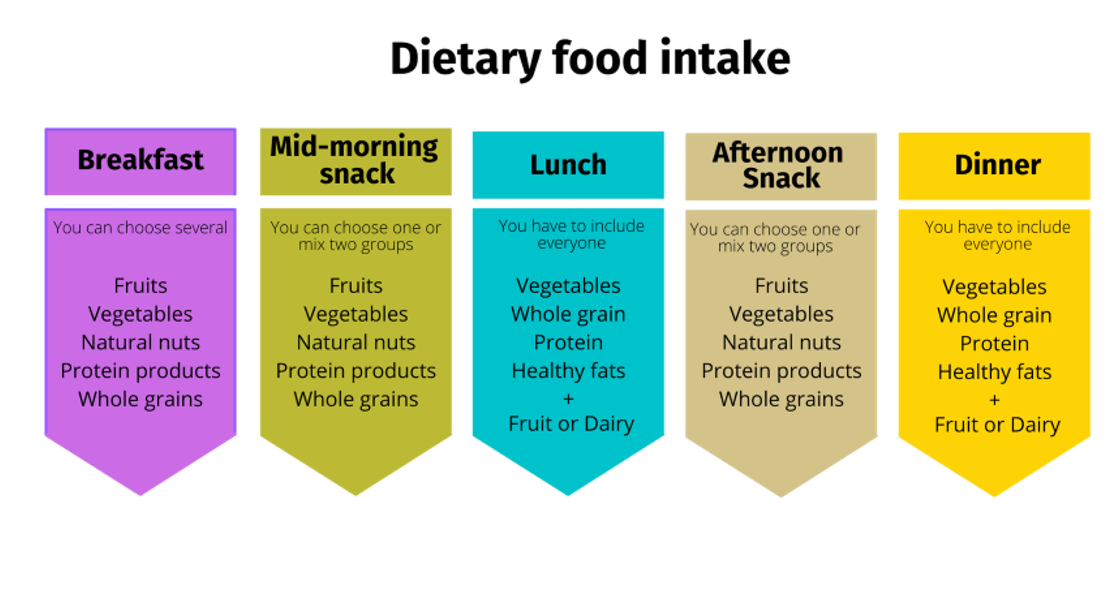
3.2.5. Balanced menu templates
The number of meals will depend on social, cultural factors or factors related to personal daily routines, always adapting to the needs and capacities of each person according to their age, state of health, pathology and other qualities that may limit intake.
Next menus are examples of a balanced diet based on before healthy eating guidelines.The texture of the food and beverages on these menus should be adapted to the needs of the person with dysphagia destined. Allergies and intolerances should also be taken into account in the menus.
Menu 1 |
|||||||
|
Monday |
Tuesday |
Wednesday |
Thursday |
Friday |
Saturday |
Sunday |
Breakfast |
Coffee with milk Toast of whole wheat bread with olive oil and turkey breast Orange |
Unsweetened Oat flakes Banana |
Oat milk Rye bread with tomato and cheese Pear |
Coffee with soymilk Banana oats hotcake with dark chocolate |
Oatmeal pourridge with cinnamon and berries |
Coffee with milk Whole wheat toast with avocado Apple |
Fruit and milk smoothie Whole wheat toast with Hummus and tomato |
Mid-Moorning snack |
Handful of nuts |
Tahini cream toast with bananas |
Yogurt |
Strawberries |
Smoothie |
Yogurt |
Handful of pistachio |
Lunch |
Lentils with vegetables Sausages Plum |
Broccoli with ratatouille Squid with aioli and whole wheat bread Yogurt |
Peas with egg and potatoes Eggplant stuffed with fish Banana |
Green beans with potatoes Lamb with potatoes Pumpkin desert |
Spaghetti carbonara Cod with bell pepper sauce Peach |
White bean salad with pickles and vegetables Turkey with apple sauce Yogurt |
Lettuce salad with corn and carrots Rice with fried tomato and egg chocolate mousse |
Afternoon Snack |
Yogurt with fruit pieces |
Yogurt |
Smoothie |
Yogurt |
Guacamole cream toast |
Smoothie with nut flour |
Yogurt with fruit pieces |
Dinner |
Cod with ratatouille Stuffed eggs Brownie with orange |
Lettuce and tomato salad Meatballs with almond sauce Pear |
House hors d'oeuvres Potato omelette with aioli and whole wheat bread Yogurt |
Baked vegetables Chicken with vegetables and tomato Roast apple with cinnamon |
Goat cheese salad on toast Beef blanquette with rice Strawberries |
White asparagus Tenderloin with pepper sauce Orange |
Sausage with rye bread Salmon with vegetables Yoghurt |
Menu 2 |
|||||||
|
Monday |
Tuesday |
Wednesday |
Thursday |
Friday |
Saturday |
Sunday |
Breakfast |
Oat milk Rye bread with avocado and olive oil Banana |
Oatmeal porridge with cinnamon and Blueberries |
Coffee with milk Toast of whole wheat bread with olive and tomato |
Coffee with milk Whole wheat toast with cheese Apple |
Coffee with soymilk Banana oats hotcake with dark chocolate |
Fruit and milk smoothie Whole wheat toast with tuna and tomato |
Unsweetened cocoa milk Oat flakes Mandarin |
Mid-Moorning snack |
Yogurt |
Smoothie with nut flour |
Guacamole cream toast |
Yogurt with fruit pieces |
Handful of almond |
Yogurt |
Smoothie |
Lunch |
Rice with fried tomato and egg Tenderloin with pepper sauce Apple |
Peas with egg and potatoes Chicken with vegetables Cheesecake |
White bean salad with pickles and vegetables Squid with aioli and whole wheat bread Strawberries |
Green beans with potatoes Sausage with rye bread Yogurt |
Chickpeas with cod Egg with béchamel sauce Pear |
Beet soup Red peppers stuffed with mince Yogurt |
Goat cheese salad on toast Tunna small turnover Greek yogurt |
Afternoon Snack |
Peanut butter and banana toast |
Yogurt with fruit pieces |
Orange |
Handful of almond |
Olive oil and tomato toast |
Pineaple |
Hummus cream toast |
Dinner |
Tomato salad with hard-boiled egg and tuna fish Sausages with potato Mandarin |
Cauliflower with garlic Steamed salmon Curd with peach jam |
Mixed salad Falafel Yogurt |
Baked vegetables Tunna omelet orange |
Pumpkin puree Meatballs with tomato sauce Orange |
Creamed spinach Moussaka Roast pear |
Spaghetti Bolognese Hake in sauce Fruit salad |
3.2.6. Preparing meals
-
Consistency or texture
This can be:
|
Source: https://cocinaycomparte.com/
|
Source: https://www.americastestkitchen.com/
|
Source: https://pixabay.com/ |
-
Blending or pureeing
If you need to blend a dry food, you will have to add a "lubricant" such as water, milk, olive oil, juice or sauce, but do not forget to check seasoning afterwards and re-thicken if necessary.
As blending food already starts off the digestion process by breaking it down, a patient can absorb much more nutrition while spending less energy on digestion.
-
Soups

Blending a soup rather than leaving "bits" still in it (even if they are soft and manageable) is far more beneficial to a dysphagic patient as it is more "filling" and helps with portion size.
Source: https://pixabay.com/
-
Seasoning and taste
Puréed or blended foods lose their taste. A dish you cook may be seasoned perfectly, but, after blending, it will taste different. The main point is to prevent food from being bland and boring. If you need to add water for the blending process, often more flavourful or spicy ingredients might be needed during cooking so that the food does not taste too diluted once blended.


Source: https://pixabay.com/
-
Colour and sauces
If a patient prefers distinct colours on a plate then please ensure each different food on the plate has the same consistency and viscosity. You then have to decide as to which dollop you are going to add the tasty sauce or gravy prior to blending, but without altering the colour.
Source:
https://orpea.es/comida-texturizada-solucion-para-los-problemas-de-alimentacion-en-personas-mayores/
3.2.7. Additional products to use
Some additional products to use to prepare meals are:
✔ Thickeners – powders and liquid;
✔ Ready-to-drink thickened drinks and drink mixes;
✔ Convenience pureed foods;
✔ Foods Mixes;
✔ Protein/calorie food enhancers;
-
Viscosity or "thickness"
Thicker (more viscous) foods are generally easier and safer to swallow than thinner foods as the risk of fluids going down "the wrong way" into the lungs is reduced.
For many, enjoying a glass of wine with friends and relatives is an important part of life and an essential part of celebrations. Many with dysphagia feel the same. We’ve therefore used our know-how creating drinks for healthcare to make alike drinks safer to swallow.
Ingredients for these are: Xanthan Gum, Maltodextrin, Erythritol.

Source: designed by Canva Pro
-
Ready-to-eat/drink products

“Baby food” for adults. They are a lot less stressful for you and the dysphagic patient who is often very embarrassed by not being able to swallow a meal you have painstakingly prepared. They are very useful to have as a supplement or standby food.
Source:https://okdiario.com/recetas/potitos-2004131
 Ready-to-drink thickened drinks and drink mixes.
They are convenient and provide proper hydration for people with
swallowing disorders. For example,
Thick-It® Clear Advantage® ready-to-drink beverages are thickened
with xanthan gum so that they have the proper consistency in order to be safe and reliable for your patients.
Ready-to-drink thickened drinks and drink mixes.
They are convenient and provide proper hydration for people with
swallowing disorders. For example,
Thick-It® Clear Advantage® ready-to-drink beverages are thickened
with xanthan gum so that they have the proper consistency in order to be safe and reliable for your patients.
Source:https://thickit.com/blog/nutrition-product-category/beverages/
-
Oral nutritional supplements
A dysphagic patient often suffers weight loss and other nutritional problems, so it is almost essential to enrich the diet in some way. Almost anything you add to any food will effectively augment its nutritional value. Although enrichment items tend to be protein based, dysphagic patients’ diet may also lack other nutrie nts.
Depending on nutritional requirements and meal replacement needs, doctors may recommend taking something more to help with the overall health and well being.
A supplement may be an individual nutrient, such as protein or fiber, or it may be a food or meal replacement, such as a fortified drink.
Oral nutritional supplements are products manufactured by the pharmaceutical industry. They are developed with the purpose of being administered to people with deficient nutritional needs. They are only prescribed by a health professional in those cases where there are nutrient deficiencies, either due to insufficient intake through diet, interaction with drugs or other causes.
In sum, the dysphagia diet may carry a large variety of supplements, but they should only be used when there are nutrient deficiencies. There are many commercial brands and different products available to people with dysphagia who require dietary supplementation. Some examples are shown in the figure below. They are not cheap, but sometimes it is a small price to pay to ensure the dysphagic patient does not become malnourished.

https://www.nestlehealthscience.es/ https://www.nutricia.es/

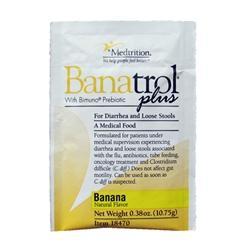

https://tesia.com.ec/hyfiber/ https://globalhp.com/shop/liquacel-liquid-protein/ https://www.nutrimedical.cl/producto/banatrol/