Unit 2 - Care and nutrition (e-book)
| Site: | IDEC TrainingCentre elearning |
| Course: | MODULE 1: METHODOLOGY AND TOOLS DEVELOPMENT FOR ADULT EDUCATORS |
| Book: | Unit 2 - Care and nutrition (e-book) |
| Printed by: | Guest user |
| Date: | Friday, 27 February 2026, 7:00 PM |
Table of contents
- Lesson 2.1. Nursing and feeding techniques and equipment
- 2.1.1. Mealtime environment: Characteristics of the place and process
- 2.1.2. Body position
- 2.1.3. Correct actions of the caregiver before, during and after feeding
- 2.1.4. Alternative feeding methods: artificial nutrition
- 2.1.5. Feeding equipment and adapted utensils
- 2.1.6. Medicine-taking
- 2.1.7. Oral care
- To know more
- Lesson 2.2. Management of oropharyngeal dysphagia. Physiotherapy a Speech-language therapy
- To know more
Lesson 2.1. Nursing and feeding techniques and equipment
What will I learn in this lesson?
The aims of this lesson is understand the importance actions during mealtime for dysphagia people, to learn about nursing and feeding techniques and equipment
Learning outcomes
To discuss the main characteristics of a safe mealtime environment.
To understand the importance of actions during mealtime for dysphagia people.
To apply the right actions of the caregiver before, during and after feeding, to discuss alternative feeding methods.
To learn about medicine-taking of patients who cannot swallow medications.
To emphasize the importance of good oral hygiene to the overall health of dysphagia patients and infection control.
2.1.1. Mealtime environment: Characteristics of the place and process
It is important to stay in a safe mealtime environment. An uninviting environment can put people off their meals and result in inadequate nutrition and hydration, while a distracting environment can reduce focus on following the strategies for safe swallowing and lead to safety concerns.
The following tips may help you to ensure the mealtime environment is optimized for the person you care for to enjoy a safe and nutritious meal:
Reduce potential distractions:
Bright, pleasant, quiet place and without noise or distractions.
Minimize the number of people walking around the meal area.
Turn off or turn down the volume on the TV, radio, mobile or tablet.
Avoid loud noises such as microwave or oven timers going off.
Brake or control of compulsive behaviors during mealtime.
Create an inviting atmosphere:
Decorating the meal area with tablecloths.
Placemats.
Plants.
Pictures and curtains can create a warm atmosphere that can help facilitate enjoyment at mealtimes.
Room and adapted furniture (chair, table, cabinets, ramps, others).
Adapted kitchenware (cutlery, glasses, plates, tablecloths, etc.) and placed on the table in an accessible and comfortable way for the diner.

Source: designed by Canva Pro
Meal time and food presentation:
The smell and appealing appearance of food can help to increase appetite as we taste not only with our tongues but our eyes and our noses as well.
Not filling the cutlery with food except in medical cases prescribed
Do not use feeding syringes or straws during oral feeding.
Establishment of a fixed schedule for all daily meals.
Maximum duration of the shots between 40-45 minutes.
After feeding, maintain a comfortable posture above 45˚ for 30-40 minutes to avoid gastric reflux.
2.1.2. Body position
Position
of a person without problems to eat.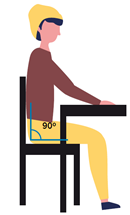
-
Back in contact with the back of the chair in a 90˚ position.
-
Head and neck aligned with the back.
-
Chin slightly inclined towards the chest.
-
Feet flat on the ground or footrest.
-
Forearms on the table on either side of the cutlery.
(Source: CADIS Huesca)
Position of a person with mobility problems.
-
Always adopt a semi-upright position above 45˚ and as close to 90˚ as possible.
-
Head slightly tilted forward, avoiding neck hyperextension.
-
Chin slightly inclined towards the chest.
-
Trunk and feet aligned with head and neck as far as possible.
-
T
 he
position of the legs will depend on the situation of the person,
alternating bent knees with straight knees and feet apart.
he
position of the legs will depend on the situation of the person,
alternating bent knees with straight knees and feet apart. -
The arms can be supported on the belly or on the armrests of the chair.
-
Cushions, pillows or other tools will be used whenever necessary to maintain proper posture.
-
Correction of posture will be made whenever necessary throughout the meal.
(Source: CADIS Huesca)
2.1.3. Correct actions of the caregiver before, during and after feeding
Before feeding, it is important to know the needs of the person and to prepare a good environment to mealtime (adapted equipment, volume, thickeners, type of texture, food temperature...).
Maintain personal hygiene by washing hands with soap and water before and after meals.
Feed meals when the person is alert and attentive; check it before starting the meal and until the end of the process. If he feels drowsy or inattentive, techniques will be done to stimulate his attention (touches on the cheeks or questions to assess his attention). If you do not manage to reach a state of adequate attention, reserve the dose for another time.
Proper positioning of the person is essential during meals. Assist him/her to sit in an upright position before feeding. If necessary, put pillows or other prop behind his back for comfort and support.
Describe what food is on the plate before mealtime
Keep calm and confident attitude during mealtime
Encourage the autonomy of each patient whenever possible.
Provide mealtime assistance when necessary
Autonomous people: supervision throughout the feeding process and support at specific times.
Dependents: supervision and support throughout the meal.
To help feed, the caregiver must position himself at the same level as the patient, normally seated nearby to one side or in front of him/her to avoid hyperextension of the neck. Avoid positions standing, behind or away.
The caregiver should give the food with his dominant arm and from the bottom up, so that the person does not raise the head.
Check the volume of the food and drink provided. Food should be lifted to the mouth in small quantities.
Clear and easy-to-understand indications about the feeding process may also be needed. This may mean giving very specific directions such as “open your mouth”, “chew”, “swallow”
If there is no response to open the mouth, visual cues can help to initiate the process of eating. This might include the caregiver opening his/her mouth or making a slight pressure on the lower lip to stimulate the opening of the mouth
If the person keeps the food in the mouth for a long time, gently rub the spoon on the lower lip to encourage mouth opening.
While person is focused on eating, there should be no distractions. Discourage conversation when there is food in the mouth.
Make sure all the food and liquid is swallowed before feeding the next bite.
Before offering sips of fluid check the mouth to make sure there is no food remaining, especially in the cavities of the cheek or on the tongue.
Never hit the teeth with utensils whilst eating.
If bite reflex occurs while the utensil is on the mouth, wait until it stops and do not force or pull the utensil to take out it.
Alternate small bites and sips. Feed the person patiently, with a slow rate of feeding.
It is vital to know signs of eating problems or risk situations that may occur during feeding and how to deal with it.
Provide a serviette or a bib during the meal and wipe the person’s mouth as needed to keep hygiene and maintain dignity.
At the end of each meal, ensure proper oral hygiene.
2.1.4. Alternative feeding methods: artificial nutrition

Enteral feeding
Enteral feeding is a method of supplying nutrients directly into the gastrointestinal tract with tube or ostomy. A person on enteral feeds usually has a condition or injury that prevents eating a regular diet by mouth, but their GI tract is still able to function. Being fed through a tube allows them to receive nutrition and keep their GI tract working. Enteral feeding may make up their entire caloric intake or may be used as a supplement.
Source: https://pixabay.com
Nasogastric (NG tube) tube is a small and special tube that goes into the stomach through the nose. Liquid food and medicines are given through the tube directly into the stomach, giving a person extra calories.
Percutaneous Endoscopic Gastrostomy (PEG) is a procedure in which a flexible feeding tube is placed through the abdominal wall and into the stomach. PEG allows nutrition, fluids and/or medications to be put directly into the stomach, bypassing the mouth and esophagus.
Parenteral nutritionParenteral nutrition (PN) or intravenous feeding, is a method of getting nutrition into your body through your veins. It include protein, carbohydrate, fat, minerals and electrolytes, vitamins and other trace elements for patients who cannot eat or absorb enough food through tube feeding formula or by mouth to maintain good nutrition status. Achieving the right nutritional intake in a timely manner can help combat complications and be an important part of a patient’s recovery. Parenteral nutrition is sometimes called Total Parenteral Nutrition (TPN). It is used in people whose digestive function is compromised or needs rest for therapeutic reasons for more than 5 - 7 days.
Videos:
Enteral feeding:
Parenteral
nutrition:
2.1.5. Feeding equipment and adapted utensils
The use of support products (instruments, equipment or technical systems that facilitate the daily activity of people with some kind of difficulty or functional limitation) during feeding to prepare, serve, eat or drink, facilitates the development of these activities but also allows the normalization of the feeding process by providing the person with greater autonomy. This has a positive impact on the establishment of social relationships, increases daily activity and improves their quality of life and therefore their self-esteem.
Cutlery
-
Good Grips Utensils /Built-Up Handle Utensils.

Enabled to assist those with limited or weakened grasping strength, the coated built-up handles help improve grasping ability and holding patterns. These non-slip utensils allow maximum control with minimum effort during mealtimes.
-
Angle cutlery with moldable handle.

For people with limited movement due to postural and other problems. The molding of the utensil allows the person to adopt the desired angle to facilitate the feeding process of the person.
-
Special cutlery.

Utensils with different shapes, designed to meet the needs of a specific population: rocking type knife, Nelson type fork or fork-spoon, ect.
-
Cutlery with soft PVC coating.

Made of aluminum but coated with food-grade PVC to make them softer, reducing the suffering of teeth for people with involuntary bite.
-
Plastic cutlery

Made of food-grade plastic, they are lighter and softer, thus reducing dental suffering in the event of bite alterations. They are light tools, can have different designs and are economically accessible.
-
Cutlery with handle and strap.

The handle has an easily adjustable strap made of cloth, plastic or other material to provide a secure grip on the utensil being used.
-
Nose Cut-Out Beaker “Nosey cup”.

This design, with its generous cut out on one side, enables drinking without tilting the head. Nose Cut Out Cup offers an easier way of drinking for anyone who struggles to tip their head back or extend their neck.
-
Two Handled Mug

Featuring two handles to be held easily increase security when you're lifting and holding your mug. The Mug also benefits from a wider base for stability and reduces the risk of spillage and prevents tipping. The mug has two handles that can be held easily o assist control. Easier to sit down and helps prevent tipping.
Reduces the risk of spillage when you are drinking from it.
-
Double-handled tumbler with spout.

Similar to the previous tumbler but with a lid to prevent the liquid from spilling completely when tipped over. It has a spout with a hole usually of about 4 mm through which the liquid falls.
-
Transparent cup with nozzle lid or without lid.

Transparent plastic cup for food use to which a lid can be fitted, which may or may not have an anti-spill system when tipped over.
-
Medela cup.

Small capacity graduated cup made of transparent plastic, with a cutout on the outside. Used for the administration of liquids to infants and babies.
Plates
-
Plates made from durable polycarbonate plastic.

Made of food-grade plastic to be light, manageability and impact resistance. A plate rim could be attached to the side of the plate to prevent food from spilling and allows the user to pick up food against the rim with one hand.
-
Manoy sloped plate.

Made from plastic, with a high back and low front, this sloped plate lets food slide towards the front, making it much easier to see and scoop up.
-
Partitioned Plate.

Made of plastic. It has features sections so that meals can be divided up. The shape of each section allows for easy scooping and makes food easier to eat.
Non-slip mat
Non-slip mats are placed under plates, cups,
cutting boards, etc. to prevent these items from slipping. Non-slip
mats are a very simple piece of equipment that can be adapted and
used in a variety of ways.
(Images source: CADIS Huesca)
There are hundreds of technical aids available on the market to facilitate any of the processes performed during feeding. Those described above are those commonly used in associations or other entities that serve people with disabilities and / or dependence.
2.1.6. Medicine-taking
Pharmacological treatment, as with the ingestion of food and beverages, requires proper handling in the mouth and coordination during swallowing.
Texture adaptation drugs is not recommended because it could be interfering with their activity, producing an overdose or limiting their effect. It is always recommended to look for other presentations of the drug before handling it.
On many occasions, it is not possible to prepare magistral formulas with other forms due to the instability of the preparation, difficulty in finding the active ingredient, etc, so in these situations the package insert should be read or the pharmacist should be asked for the best way to adapt it.

(Source: https://www.freepik.com)
To select the most appropriate pharmaceutical form will be made according to the type of dysphagia:
- Dysphagia to liquids. Choice of medication in tablet or capsule form. They can be administered together with thickened liquids with the appropriate texture.
- Dysphagia to liquid and solid food. Semi-solid textures are recommended, and depending on the person's capabilities, they can be administered together with a small part of the food or not.
Take precautions when administering and choose the most appropriate one. Modification of its texture should be avoided. In case it is not possible, find out if it is possible to crush it without alteration.
- Semi-solid textures are recommended and depending on the person's capabilities. They can be administered together with a small part of the food or not.
- The medicine has to be included in the first spoonfuls of the food. It is not recommended to mix with all food content because it modifies the taste and may not be completely consumed, diminishing its effect.
- It is not recommended to administer
together with citric juices or yogurts because they increase salivation,
increasing the risk of aspiration.
- An alternative to medicines that cannot be administered with food is the use of gelatines and thickeners.
- Hight fluid drugs are recommended to
dilute them first in a small amount of water (10-15ml) and then add a
thickener.
- Laxatives are recommended to thicken them with a new generation thickener with food gums.
- Rectal route is a valid procedure to
administer medication in suppositories or enemas.
- The dosed transdermal patches are also rapidly absorbed and they are not recommended in case of skin problems.
● Dysphagia to solid meals. The options are:
- Liquid forms: oral solutions, syrups, drops, sachets for reconstitution and in some situations injectables that can be administered orally.
- Effervescent tablets: they should be dissolved in little water (20 ml approx.). It is necessary to wait for the effervescence to disappear as it can be irritating and cause coughing, which is a risk during swallowing.
- Orodispersible tablets: called "Flas, Liotabs or dispersible". They dissolve on contact with saliva and do not require the use of external liquids for dissolution.
- Sublingual tablets: they should not be swallowed but allowed to dissolve under the tongue.
Non-crushable medicines
Not all tablets can be crushed without alterations. In general only uncoated tablets should be crushed and only uncoated hard gelatin capsules should be opened. Once crushed or opened, the dosage form should be mixed with a small amount of soft food or gelled water and administered immediately. The capsules are formulated so that the gelatin capsule facilitates swallowing and masks the unpleasant taste of the drug, including laxative substances.

Source: designed by Canva Pro
Modified release dosage forms:
They are formulations where the rate and/or site of release of the active ingredient(s) are different from that of the immediate release dosage form administered by the same route. Modified release dosage forms covered by this guideline include orally, intramuscularly, subcutaneously administered modified release and transdermal dosage forms.
Prolonged release dosage forms: prolonged release dosage forms are modified release dosage forms showing a sustained release compared to that of an immediate release dosage form administered by the same route.
Delayed release dosage form: The release of the active substance from such modified release dosage forms is delayed for a certain period after administration or application of the dosage. The subsequent release is similar to that of an immediate release dosage form.
Multiphasic release dosage forms:
- Biphasic Release: the first phase of drug release is determined by a fast release dose fraction providing a therapeutic drug level shortly after administration. The second extended release phase provides the dose fraction required to maintain an effective therapeutic level for a prolonged period.
- Pulsatile Release: Pulsatile drug release is intended to deliver a burst of drug release at specific time intervals.
Multiple-unit: A multiple unit dosage form contains a plurality of units e.g. pellets or beads each containing release controlling excipients, e.g. in a gelatine capsule or compressed in a tablet.
Single-unit: The single-unit dosage forms consist of only one unit, e.g. Osmotic tablet.
Intramuscular/subcutaneous depot formulations: A depot injection is usually a subcutaneous or intramuscular product which releases its active compound continuously over a certain period of time. Subcutaneous depot formulations include implants.
Transdermal drug delivery systems (TDDS): A TDDS or transdermal patch is a flexible pharmaceutical preparation of varying size containing one or more active substance(s) to be applied on the intact skin for systemic availability.
Keep in mind
Mainly drugs are administered during lunch and/or dinner, so it is important to know:
When it is essential to crush a drug, the final product must be homogeneous. In addition, the use of spoons and mortars should be avoided or cleaned thoroughly after each trituration.
Medications, as well as food and beverages, can also give rise to aspirations leading to choking, respiratory infections and even cardiorespiratory or other arrests.
To include the medication in the first spoonful of the food or drink to consume it all and that it does not contribute strange or unpleasant flavors.
Do not use citrus juices or yogurts with the medication since salivation is increased and the risk of aspiration is accentuated.
Use gelatins, thickeners or starches for medications that cannot be administered with food.
Drugs with a high fluidity should be diluted in a small amount of water (10-15ml) and then a thickener should be added until the appropriate texture is obtained.
Sedatives can thicken the saliva and may hinder the swallowing process.
Laxatives can be administered by dissolving in water and with new generation thickeners.
Rectal and transdermal routes are a valid way of administering drugs by means of suppositories or enemas. Rectal absorption is good as it is a very vascularized area.
Transdermal patches are also rapidly absorbed. They are not recommended when skin problems exist.

Source: designed by Canva Pro
Therefore, people with dysphagia should avoid any drug not indispensable and choose the correct form when it is. Moreover, oral solution, rectal or transdermal, should be considered.
2.1.7. Oral care
Why is oral care important?
Oral care is essential for everyone to maintain clean and healthy teeth and mouths. However, people with dysphagia (difficulty with chewing and swallowing) are at a greater risk of poor oral hygiene and health.
This is because they are at risk of food and drink pooling in the mouth and inhaling food, drink and saliva into the lungs (aspiration) when swallowing. Aspiration of the harmful bacteria that develops in unclean mouths can lead to life threatening respiratory difficulties and chest infections known as aspiration pneumonia.

(Source: https://www.freepik.com)
How often should oral care be performed?
Oral care should be performed at least twice a day morning and night, but people with dysphagia may need extra oral care before and after meals. This is to minimise their risk of aspirating harmful bacteria and any fluid that may be pooling in the mouth.
It is also important to remove any food debris from the teeth and mouth after meals that could pose a choking risk. Debris also provides a breeding ground for bacteria and the development of plaque that leads to tooth and gum disease.
Who should perform oral care?
Wherever possible the person should be encouraged to brush their own teeth. This may be difficult for people who find it difficult to hold a toothbrush. There are toothbrushes which have large handles and angled heads to make them easier to use.
Alternatively, you may need special handgrips and other adaptations which can be fitted to manual toothbrushes to make them easier to hold. Electric toothbrushes with oscillating heads are very effective at providing a large amount of cleaning action with very little movement needed from the user, although you do need to position the brush correctly.
What products should I use?
a dry small headed soft to medium bristled toothbrush;
a small pea-sized amount of toothpaste on a dry toothbrush.

(Source: pixabay.com)
How to perform oral care for those who need help?
If the person requires assistance to perform oral care you should:
stand or sit behind them because it helps to support their head and means your hands are in the most appropriate position to brush their teeth
Tilt the persons head forward slightly to reduce their risk of aspirating on the toothpaste and debris brushed from their teeth
Aim to lay them on their side with their head on a pillow and a towel covering the pillow if the person is unable to sit upright
do not wet the toothbrush which will keep foaming to a minimum.
What if the person is nil by mouth (NBM)?
Some people with severe dysphagia are unable to be fed orally and are fed via a feeding tube. It is important that their teeth and mouths are kept clean and healthy.
Sometimes people who are NBM can form calculus more quickly and it may be difficult to remove. Good tooth brushing will prevent this.
They may develop aversion or ‘sensory defensiveness’ to oral care. This can be avoided with very gradually increased amounts of regular oral care with a soft toothbrush and mild or unflavoured toothpaste. People who are nil by mouth frequently suffer from dry mouth.
What if the person suffers from dry mouth?
Oral care is especially important for individuals who suffer from dry mouth as they are at greater risk of dental decay and gum disease. A dry mouth is very uncomfortable and also makes chewing and swallowing more difficult.
If able the person should be encouraged to take frequent sips of water. There are also a number of saliva substitute gels and sprays designed to provide moisture and comfort.
What if the person wears dentures?
Oral care is equally important and night, and rinsed after eating to remove any debris. When removed, all surfaces of the people with no natural teeth to keep the mouth clean, healthy and to promote saliva flow. Dentures should be removed at night to allow the gums to rest. They should be cleaned twice a day, morning dentures should be brushed with a toothbrush or denture brush to remove any plaque and debris.
Dentures can be brushed with warm soapy water; a denture cleanser will help to remove stubborn stains. Ensure you clean dentures over a sink filled with water in case you accidentally drop them. When not in the mouth they should be left to soak in cold water to prevent them warping and cracking.
Oral hygiene recommendations based on dysphagia severity and common speech-language pathology interventions
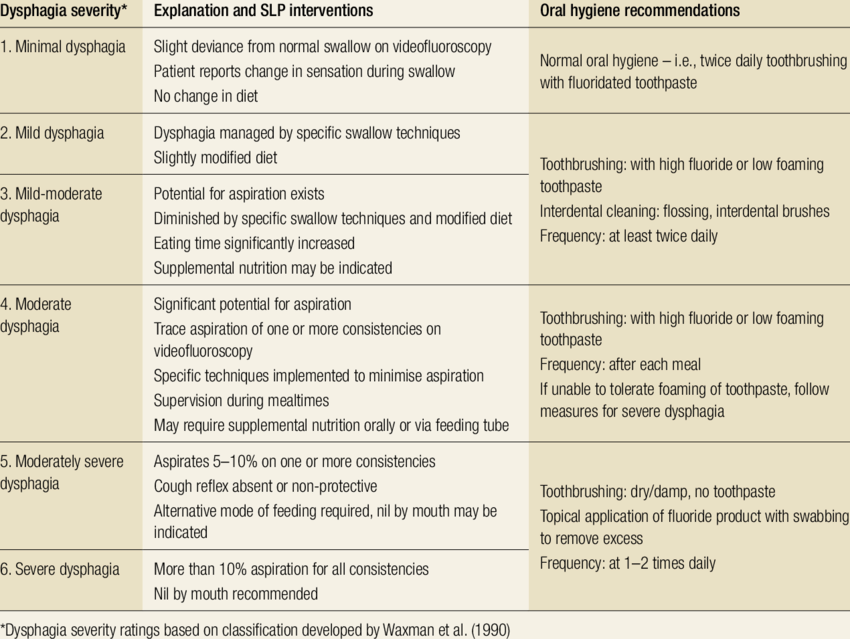
Obtained from: Lim M. Basic oral care for patients with dysphagia - A Special Needs Dentistry perspective. JCPSLP. 2018; 20(3):142-9.
To know more
- Cortés AC.Comer diferente, comer bien: recetas seguras para chuparse los dedos. Recetario de alimentos texturizados. CADIS Huesca. 2020:1:1-223.
- Guideline on the pharmacokinetic and clinical evaluation of modified release dosage forms (EMA/CPMP/EWP/280/96 Rev1). 2014. Available at: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-pharmacokinetic-clinical-evaluation-modified-release-dosage-forms_en.pdf
- Lim M. Basic oral care for patients with dysphagia - A Special Needs Dentistry perspective. JCPSLP. 2018; 20(3):142-9.
- Clinical Guidelines (Nursing) for enteral feeding and medication administration. Available at: https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Enteral_feeding_and_medication_administration/
- Enteral Feeding: How It Works and When It’s Used. Available at: https://www.healthline.com/health/enteral-feeding#procedure
- What Is Parenteral Nutrition?. Available at: https://www.nutritioncare.org/About_Clinical_Nutrition/What_is_Parenteral_Nutrition/
Lesson 2.2. Management of oropharyngeal dysphagia. Physiotherapy a Speech-language therapy
What will I learn in this lesson?
The aim of this lesson is to learn safe swallowing procedures that can be used to improve dysphagia treatment by speeding up the recovery of swallowing function and reducing hazards.
Learning outcomes
To understand patients' use of safe and alternate techniques to maintain eating and drinking functions.
To recognize the benefits of these techniques in the treatment of dysphagia.
To learn swallowing exercises which may help to improve and/or maintain swallowing functions.
2.2.1. Safe swallowing techniques
Food, fluids, and saliva must be transported from the mouth through the throat and into the stomach in a timely and coordinated manner.
When someone has a swallowing problem (dysphagia), it runs the risk of food, water, and saliva getting into the lungs (aspiration). It's possible that the person is completely unaware of what's going on (silent aspiration).
Aspiration can lead to pneumonia, which is hazardous. Choking is also a possibility for people suffering from dysphagia.
There are some ways for keeping patient safe while eating and drinking:
Take a sip of your beverage, then look down at your lap before swallowing.
Take a sip of your drink after each bite of a meal.
Hold each mouthful and sip for 3 seconds in your mouth before swallowing. Turn your head and swallow after each mouthful and sip.
Take a small drink and swallow, pause, and cough while holding your breath. When you eat or drink something, sit bolt upright.
After eating, sit upright for at least 30 minutes.
Clear your throat hard after each swallow and swallow again. Clear any remnants in your mouth with your tongue.
When drinking from a cup, use a straw to avoid tipping your head back.
Crush your medications and put them in anything like apple sauce, yogurt, or pudding as a carrier.
When you have food in your mouth, try not to speak.
2.2.2. Alternate techniques of swallowing
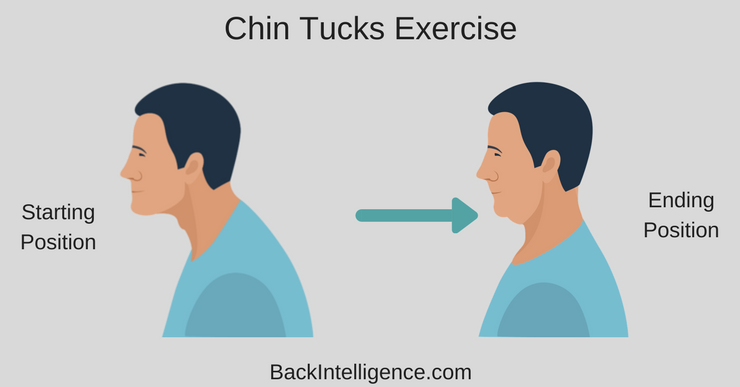
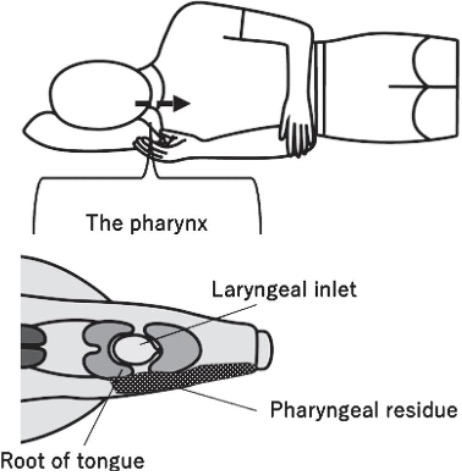
Chin Tuck
To shift the bolus anterior, lower your chin. It reduces early spilling by widening the valleculae, which causes spillage to pause, giving the VFs more time to close, minimizing the likelihood of aspiration.
Source: https://backintelligence.com

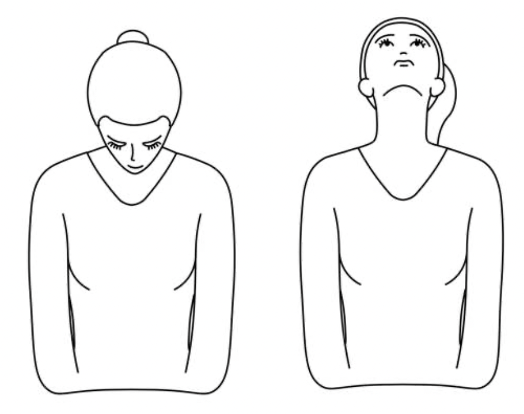
Head tilt
When you turn your head to the better side, the bolus is redirected through the oral canal, which improves oral bolus transport.
Source: https://www.vhdissector.com
Head Rotation
Twist the head to the weaker side, closing off the weaker side and allowing the bolus to pass to the stronger side. Pocketing is also avoided.
Rotating the head to the left or right increased pharyngeal contraction pressure at the level of the valleculae and pyriform sinuses on the side of rotation, decreased UES resting pressure on the side opposite rotation, and increased the duration from peak pharyngeal pressure in the pyriform sinuses to the end of UES relaxation when compared to a neutral head position and The anterior-posterior opening diameter of the UES has been enlarged.
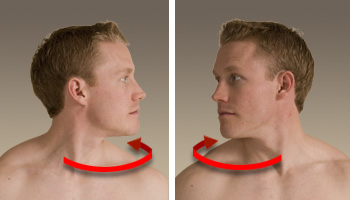
Source: https://www.vhdissector.com
Side Lying
The prevailing rationale for using the side-lying approach is that lying down will keep remaining bolus material attached to the pharyngeal walls rather than allowing it to fall into the airway, which could happen more easily in an upright position due to gravity.
Source: Kaneoka A, Inokuchi H, Sakai T, Saito Y, Haga N. Utility of Side-lying Posture in a Patient with Severe Dysphagia Secondary to Oropharyngeal Cancer Surgery: A Single Case Report. ACS. 2022;25(1): 29-36. doi: 10.3233/ACS-210039
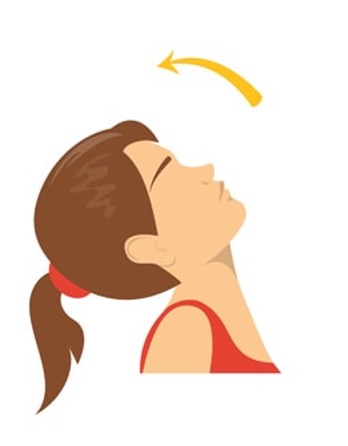 Head Back
Head Back
Utilize gravity to cleanse the oral cavity and bypass the oral stage.
Source: https://northernmyotherapy.com.au/
Neck extension
The individual is encouraged to sit or stand erect in the neck extension posture and to extend the neck backwards and elevate the chin upwards when transferring the bolus from the oral cavity to the pharynx.
Source: https://www.istockphoto.com
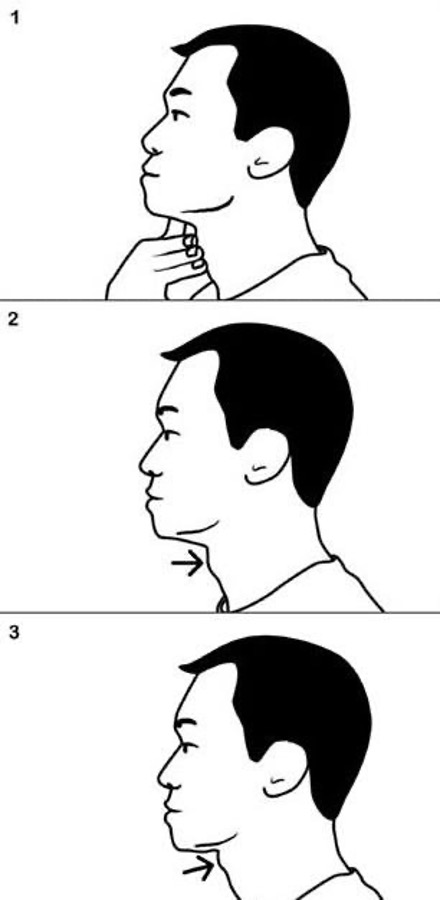
Mendelsohn manoeuvre
The Mendelsohn manoeuvre is used to treat laryngeal melevation during swallowing. This maneuver necessitates a person with excellent cognitive talents. The individual is told to keep the swallow at the height of vertical larynx movement.
Source: Григус, І & Mykola, R. Clinical review of physical therapy intervention of swallowing disorder after stroke. 2013.
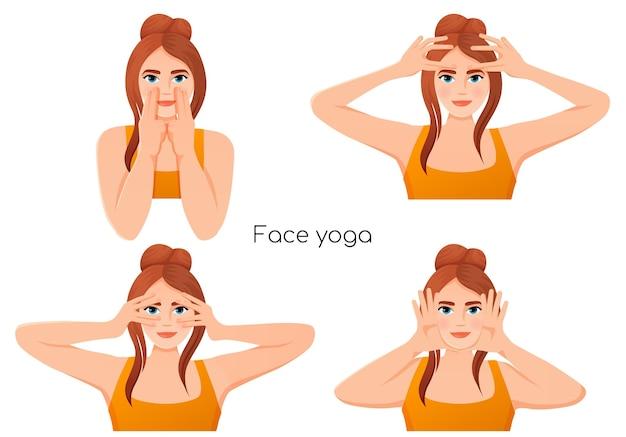
2.2.3. Swallowing exercise
What can we do to avoid swallowing difficulties?
When we swallow, we use 30 distinct muscles. It is critical to maintain these muscles active during treatment by continuing to eat and performing swallowing exercises both during and after treatment. These exercises will help people suffering from dysphagia stretch and strengthen their mouth and throat muscles.
Professionals involved in dysphagia management may select the most appropriate exercises for patients and show them how to do these exercises.
Useful tips to make swallowing exercises
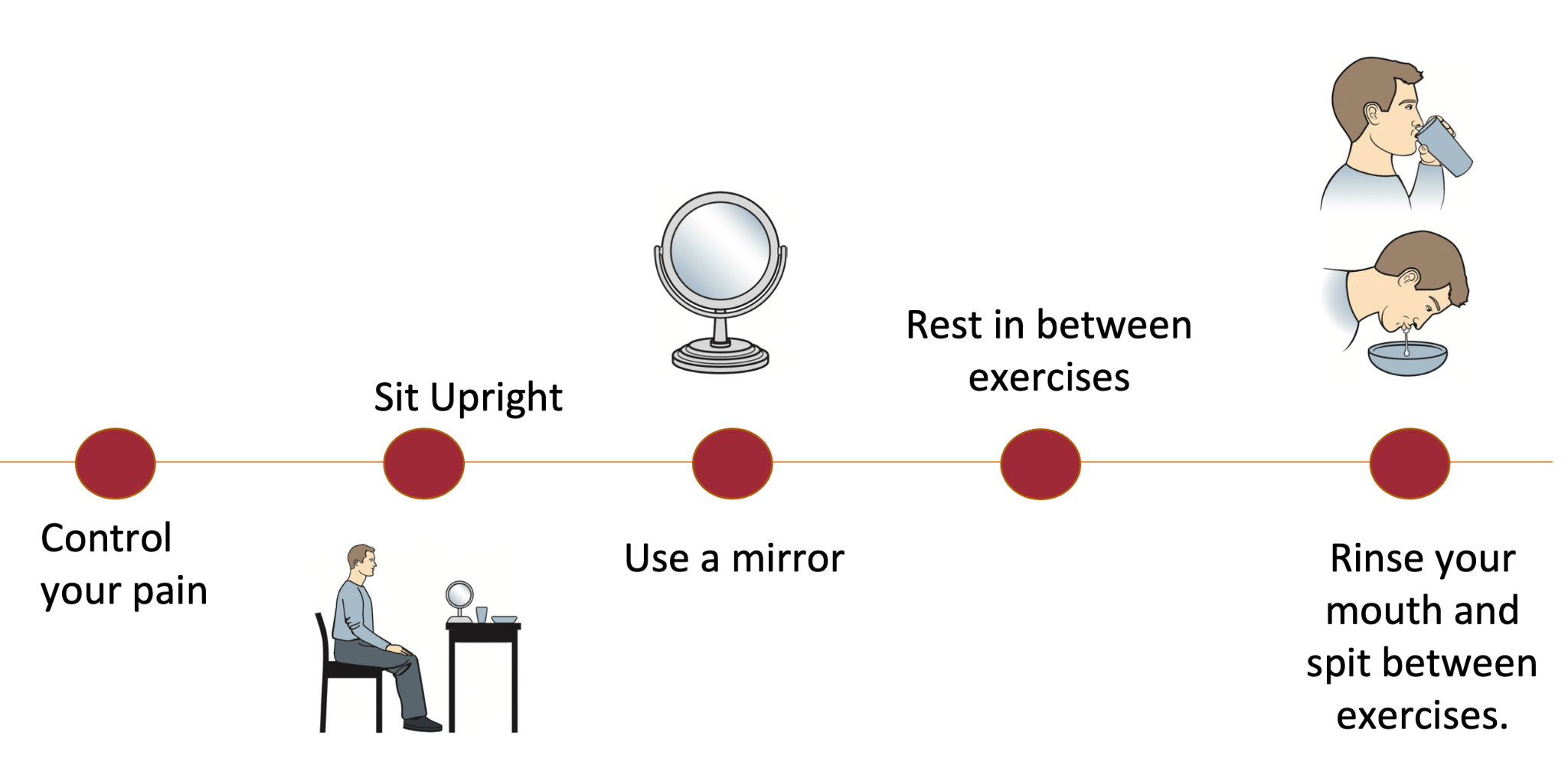
Source: University Health Network (www.uhn.ca)
Exercise 1: The Effortful Swallow
To make your throat muscles stronger. If you're eating by mouth, repeat this activity after each bite of food.
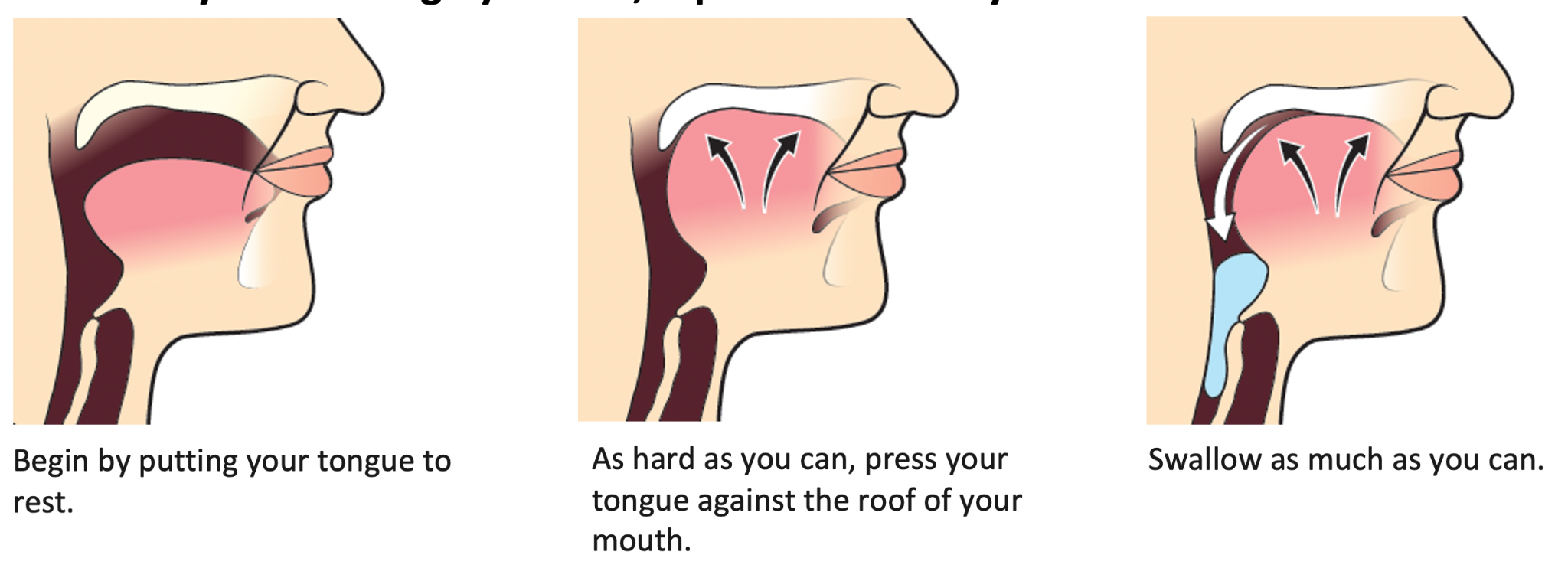
Source: University Health Network (www.uhn.ca)
Exercise 2: The Masaco Technique
To make your throat muscles stronger.
Hold the tip of your tongue between your teeth or your lips. Try to swallow your spit while keeping your tongue in place.
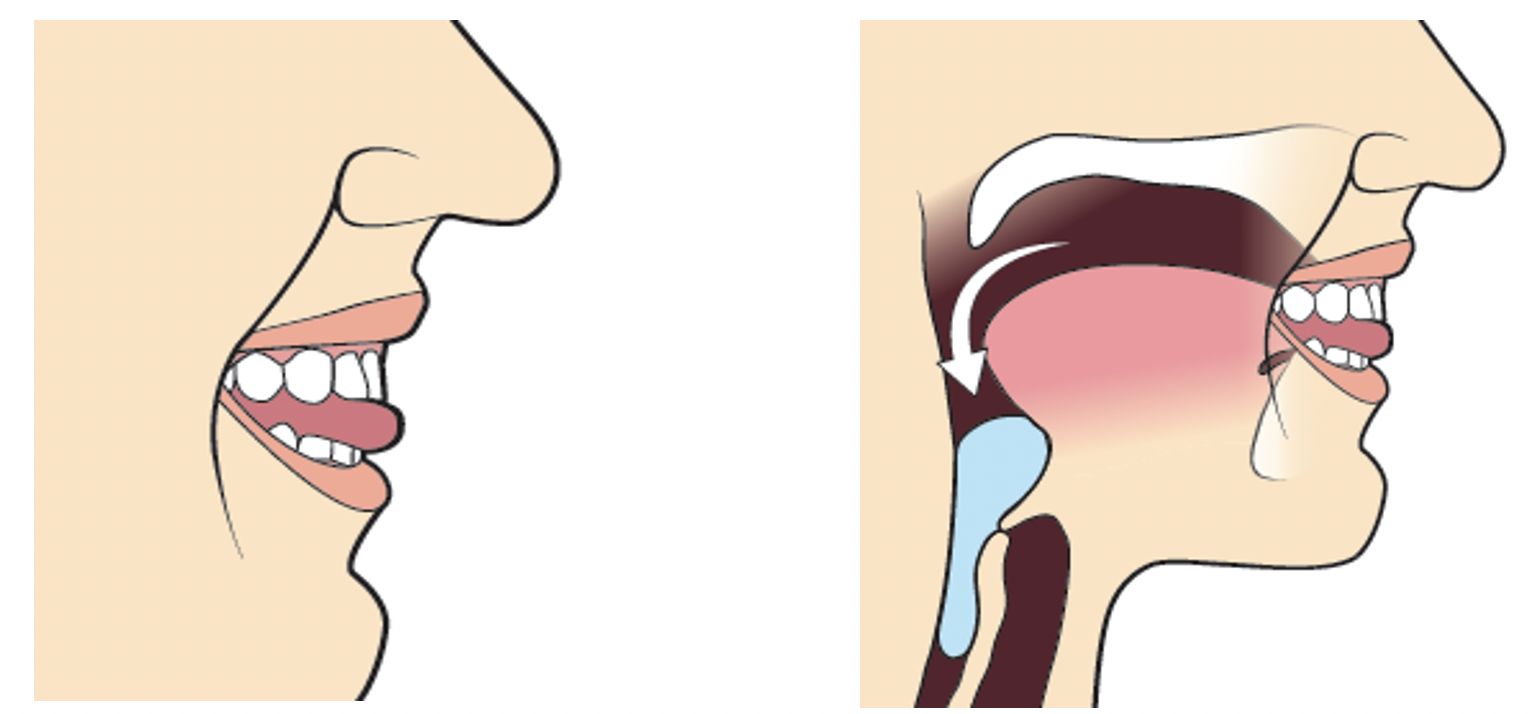
Source: University Health Network (www.uhn.ca)
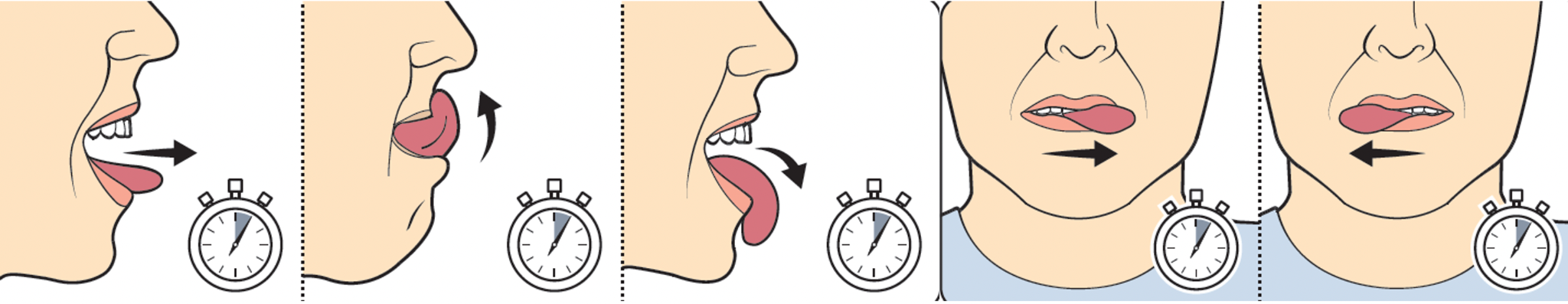
Exercise 3: Range of Motion Exercise (Jaw)
To stretch the muscles in your jaw.
Make your mouth as big as possible. Hold the position for 5 seconds. Make a right-hand movement with your jaw. Hold the position for 5 seconds. Make a left-hand movement with your jaw. Hold the position for 5 seconds.
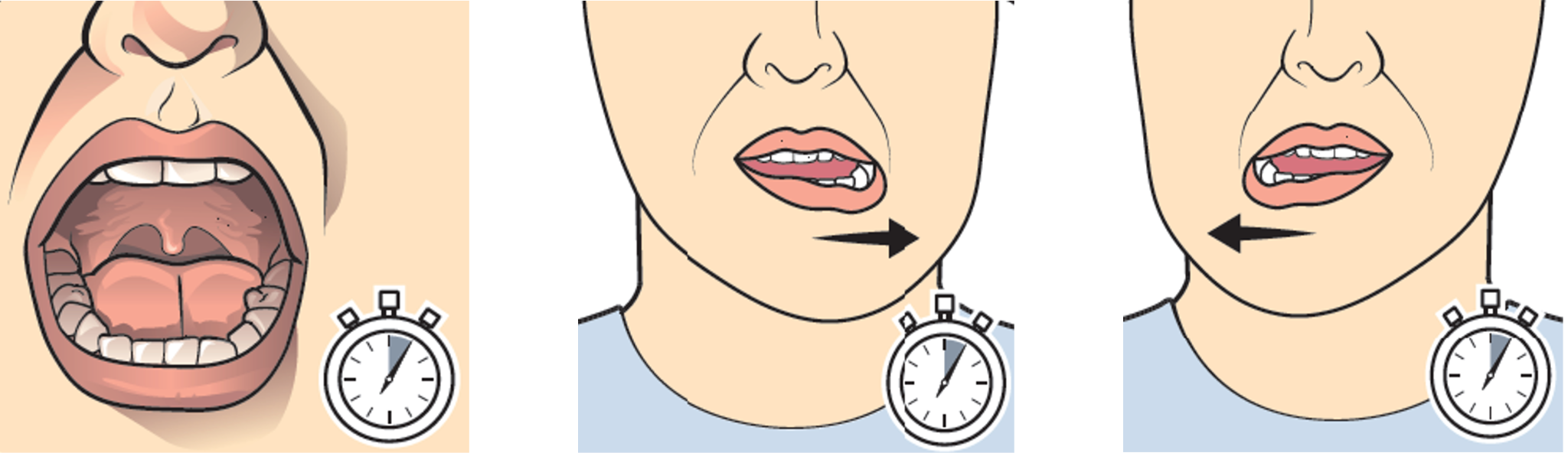
Source: University Health Network (www.uhn.ca)
Exercise 4: Range of Motion Exercise (Tongue)
To stretch the muscles in your tongue.
Extend your tongue as far as it will go. Hold the position for 5 seconds. Raise your tongue to the bridge of your nose. Hold the position for 5 seconds. Make a downward motion with your tongue towards your chin. Hold the position for 5 seconds. Make a left-hand movement with your tongue. Hold the position for 5 seconds. Make a right-hand movement with your tongue. Hold the position for 5 seconds.
Source: University Health Network (www.uhn.ca)
Exercise 5: The Supraglottic Swallow
To keep your air clear.
Source: University Health Network (www.uhn.ca)
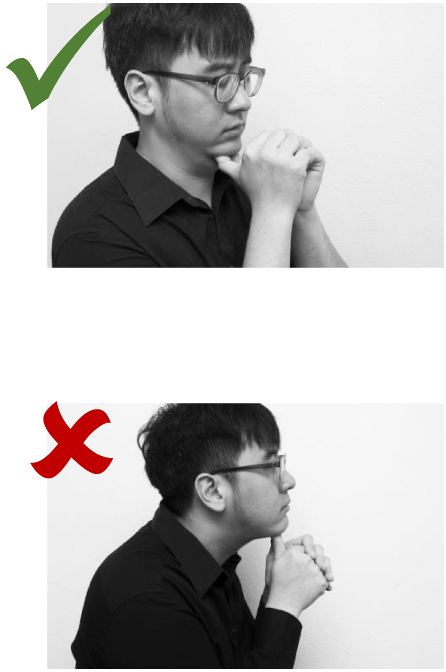
Exercise 6: Modified Shakers Exercise
-
Sit up straight and breathe deeply.
-
Place your thumbs beneath your chin.
-
Tuck your chin between your thumbs.
-
Keep your hands in place for one minute. Repeat this process three times more.
-
Hold for one second, then repeat 30 times.
Note: You should be able to feel the front of your neck exercising. There should be no discomfort in the back of your neck. REMEMBER NOT TO PUSH YOUR HEAD FORWARD.
Source: Swallowing Exercises for head and neck radiation therapy. Singapore General Hospital (https://www.sgh.com.sg/)
Tongue Base Strengthening Exercises
The base of your tongue is important for creating pressure that helps in swallowing. These workouts will strengthen and improve your tongue base's movement. Some persons who have difficulty swallowing may benefit from these exercises.
You should avoid doing these exercises with food in your mouth.
-
Gauze Exercise: Between your front teeth, place a rolled piece of gauze. Hold the gauze in place gently and swallow.
-
Gargle Exercise: Pull your tongue back as far as you can in your mouth. Pretend to gargle vigorously, then exhale.
-
Tongue Pull-Back: Pull your tongue back into your mouth as far as possible by sticking it straight out. Hold the position for 2 seconds.
-
Yawn: For 1 second, yawn and open your mouth as wide as you can.
Tongue Exercises
-
Open-Mouth Swallows: While keeping your lips open, take a deep breath and swallow quickly.
-
Tongue Protrusion: Stick your tongue as far as possible out of your mouth without touching your lips. Keep it there for 3-5 seconds.
-
Tongue Retraction: As though you're ready to create a "kuh" sound, pull the base of your tongue back down your neck until it contacts the throat wall. Hold the position for 3-5 seconds.
-
Tongue Retraction/Protrusion: Combine the two previous exercises. Hold each for a couple of seconds.
-
Gargle: Make a gargle sound by pulling your tongue back into your throat. Hold for a couple of seconds.
-
Tongue Lateralization: Make your tongue protrude out by pressing it hard on the inside of your cheek. For 3-5 seconds, press your index finger against your tongue through your cheek. Rep on the opposite side.
-
Tongue Press: For 3-5 seconds, press your tongue against the roof of your mouth as hard as you can.
-
Tongue Sweep: Place the tip of your tongue behind your upper teeth. Return your tongue tip to the roof of your mouth slowly but firmly.
-
Tongue Circles: Your tongue should be firmly pressed on the inside of your lips. Slowly make a circle to the right, then to the left.
-
Teeth Counting: Slowly touch and count each of your teeth with the tip of your tongue.
Throat Exercises
-
Pitch Glides: Sing “ee” starting at the lowest note and slowly slide up the scale to your highest note. Hold for 10-20 seconds.
-
Shaker (Part 1): Lie on your back without a pillow. Lift your head up and look at your toes. Hold for 30 seconds, then rest for 30 seconds. Repeat 3 times.
-
Shaker (Part 2): Lie on your back without a pillow. Lift your head up and look at your toes. Quickly relax your head. Repeat 30 times.
-
Valsalva: Say “hut” firmly, then swallow right after.
-
Towel Tuck: Place a rolled hand towel between your neck and chest. Tuck your chin and hold the towel in place without using your hands. Swallow hard.
2.2.4. Exercises for cheek muscles
What is the exercise for cheek muscles?
 Your cheek muscle workouts will be determined
by the nature of your swallowing problem. You might have trouble with
the first step of swallowing, before the food stuff leaves your
mouth, for example. If this is the case, training the muscles in this
area may be beneficial.
Your cheek muscle workouts will be determined
by the nature of your swallowing problem. You might have trouble with
the first step of swallowing, before the food stuff leaves your
mouth, for example. If this is the case, training the muscles in this
area may be beneficial.
How can we do it?
These exercises can be done in your hospital room or at home. You can usually do these
exercises on your own, but you can also work with a health expert.
Among the exercises for strengthening the cheek muscles are:
Filling the cheeks with air and retracting them,
Moving air from one cheek to the other
Workouts that strengthened the tension in the cheek muscles (resistance attempt against the expansion of the cheek with a spatula placed in the vestibule).
These exercises are done a total of ten times.
To know more
Bath PM, Lee HS, Everton LF. Swallowing therapy for dysphagia in acute and subacute stroke. Cochrane Database Syst Rev. 2018 Oct 30;10(10):CD000323. doi: 10.1002/14651858.CD000323.pub3.
Carnaby-Mann G, Crary MA, Schmalfuss I, Amdur R. "Pharyngocise": randomized controlled trial ofpreventative exercises to maintain muscle structure and swallowing function during head-and-neckchemoradiotherapy. Int J Radiat Oncol Biol Phys. 2012 May 1;83(1):210-9. doi: 10.1016/j.ijrobp.2011.06.1954.
Kagaya H, Inamoto Y, Okada S, Saitoh E. Body Positions and Functional Training to Reduce Aspiration in Patients with Dysphagia. JMAJ. 2011;54(1): 35–38.
Kotz T, Federman AD, Kao J, Milman L, Packer S, Lopez-Prieto C, Forsythe K, Genden EM. Prophylacticswallowing exercises in patients with head and neck cancer undergoing chemoradiation: a randomized trial. Arch Otolaryngol Head Neck Surg. 2012 Apr;138(4):376-82. doi: 10.1001/archoto.2012.187.
Messing BP, Ward EC, Lazarus CL, Kim M, Zhou X, Silinonte J, et al. Prophylactic Swallow Therapy forPatients with Head and Neck Cancer Undergoing Chemoradiotherapy: A Randomized Trial. Dysphagia. 2017 Aug;32(4):487-500. doi: 10.1007/s00455-017-9790-6.
Suman Z. Effectiveness of Swallowing Exercises in Dysphagia: A Speech-Pathologist Perspective [PhD Thesis] University of Health Sciences Lahore. 2015.
Dysphagia and safe swallowing. Available at: https://www.independentnurse.co.uk/clinical-article/dysphagia-and-safe-swallowing/86310/;2015
Swallowing Exercises. University Health Network. 2022. Available at: https://www.uhn.ca/PatientsFamilies/Health_Information/Health_Topics/Documents/Swallowing_Exercises_for_Patients_with_Head_and_Neck_Cancer_Receiving_Radiation_Treatment.pdf
Swallowing Exercises Handout and 21 Compensatory Strategies. Available at: https://thehomehealthslphandbook.com/dysphagia-series-swallowing-exercises-strategies-free-patient-handout/
Swallowing Exercises for head and neck radiation therapy. Singapore General Hospital. Available at: https://www.sgh.com.sg/patient-care/specialties-services/Speech-Therapy/Documents/DRO%20Handout%20(Eng).pdf
Tongue Base Strengthening Exercises. Available at: https://www.healthinfotranslations.org/pdfDocs/TongueBaseExer.pdf
Speech and Swallowing Exercises. Huntsman Cancer Institute - University of Utah. 2022. Available at: https://hci-portal.hci.utah.edu/sites/factsheets/Shared%20Documents/speech-and-swallowing-exercises.pdf?Mobile=1