Unit 1 - Dysphagia (e-book)
| Site: | IDEC TrainingCentre elearning |
| Course: | MODULE 2: CAREGIVERS, FAMILIES AND PEOPLE WITH DYSPHAGIA |
| Book: | Unit 1 - Dysphagia (e-book) |
| Printed by: | Guest user |
| Date: | Friday, 6 February 2026, 12:25 PM |
Description
1.1 Swallowing
1.1.2 Swallowing phases
|
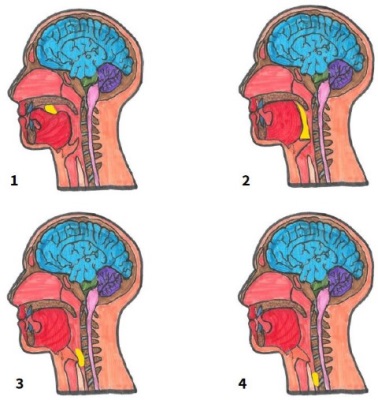
Swallowing is divided into three stages:
|
Figure 1. Swallowing mechanism (Source: CADIS Huesca) |
|---|
Practical exercises to apply the theory.
In this exercise we will be aware of the swallowing process.
Materials: a fruit ready to eat
Steps to follow while being aware of the process:
1- Take the fruit and introduce it in the mouth. Observe how the mouth opens and the teeth help to cut the food into a small part that will remain inside the mouth.
2- Chew the food and form the food bolus. In this phase notice how the food is chewed and with the help of the tongue it is thrown from one side of the mouth to the other and unites with the saliva.
3- Group all the food in the mouth at the base of the tongue. Notice the movements of the mouth and how the tongue helps you to group them.
4. Swallow the food bolus. Observe how there is a rapid movement of the tongue that pushes the food into the throat.
5. Finally, the last two phases of swallowing happen very quickly. Observe how the food passes through the duct that communicates the mouth with the stomach.
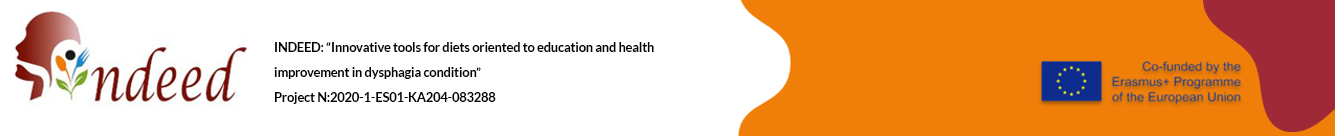
Figure
2. Infographic of swallowing (Source: designed by Canva Pro).
Infographics available for download on the training platform (https://indeed-project.org/)
1.2 Dysphagia
1.2.1 Overview
Occasional difficulty swallowing, which may occur when you eat too fast or don't chew your food well enough, usually isn't cause for concern. However, If these complications are frequent, they may indicate a serious health problem that requires treatment. Many of these medical complications can be to dysphagia.
About 8% of the world's adult population has dysphagia. In certain cases, this percentage is even higher;
• 20-60% in people over the age of 55.
• 35-84% in neurological disease (Parkinson (35-50%), Alzheimer (84%), ELA (60%) …).
• 20-80% other medical situations (impact, surgery or cancer).
1.2.2 Definition of Dysphagia
Dysphagia is the difficulty or sensation of having difficulty swallowing certain foods, liquids, medicines or saliva.
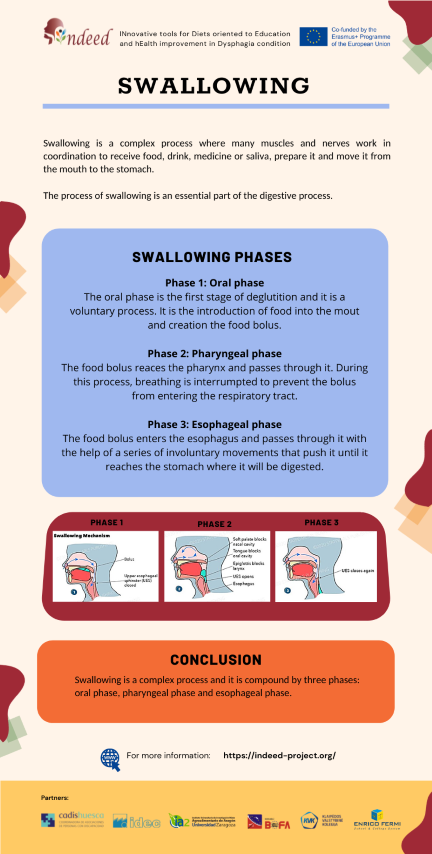
Difficulties can occur in any of the three phases of swallowing. It can be classified according to the location of them.
 |
 |
 |
|---|---|---|
| Go
video: Dysphagia videofluoroscopy (Ianessa humbert, 2020) |
Go
Video: Explanation about Dysphagia (Cadis huesca, 2021) |
Go Video:
Difficulty Swallowing (freemededucation, 2018) |
1.2.3 Dysphagia classification
Dysphagia can be broken down into two main classifications according to the place where they take place: Oropharyngeal dysphagia and Esophageal dysphagia.
Oropharyngeal dysphagia. Problems occur during one of the first two stages of swallowing. There is a failure at some point in the coordinated swallowing process.
Esophageal dysphagia. Problems occur during the last phase of swallowing Patients usually describe symptoms of food getting stuck seconds after initiating swallowing and identify it occurring in the upper half of the thorax or slightly lower.
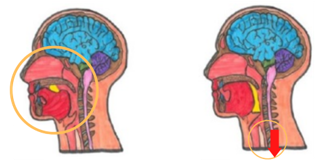
Figure 3. Disphagia classification (Source: CADIS Huesca)
1.2.4 Most frequent signs and symptoms
- Difficulty picking up food from the cutlery
- Increased time chewing and oral handle
- Inability to keep the bolus in the oral cavity
- Difficulty performing and coordinating oral movements with the facial, oral and lingual muscles
- Loss of strength during chewing
- Excessive chewing pattern
- Hesitation or inability to initiate swallow
- Difficulty when initiating to swallow with or without pain
- Prolonged eating time
- Frequent repetitive swallows
- Drooling.
- Food residue in the mouth after swallowing
- Pain, discomfort or a feeling of stuck in the throat
- Sweating, watery eyes and discomfort
- Nasal or oral regurgitation
- Changes in tone of voice, hoarseness or wet voice or nasal
- Frequent choking
- Airway obstructions
- Feeling of choking when swallowing
- Nausea or vomiting
- Reflux
- Sensation of food getting stuck in the throat or chest, or behind the breastbone.
- Recurrent respiratory infections
- Cough during meals or up to 20 minutes later
- Recurrent fever or low-grade fever
- Color change in the fingers or lips
- Weight loss
- Dehydration
Practical exercises to apply the theory.
In this exercise we will identify signs of dysphagia in a person during the feeding process.
Timetable: apply during mealtime
Materials: food prepared for that meal.
Steps to follow being aware of the process:
1- Situation. Sit in a chair next to the person with suspected dysphagia, at the same height but without interfering in the process or making the person uncomfortable.
2- Observation of the process. from the moment he/she picks up the spoon from the table, picks up the food with the mouth, chews it, forms the bolus, swallows it and even finally wipes the mouth at the end.
3- Identification of signs. Be alert to identify if any sign occurs in any of the steps during feeding.
Note: if we do not have a person to observe, we can do it with ourselves by eating or remembering a meal with a person we suspected to have dysphagia.

Figure 4. Infographic of dysphagia. (Source: designed by Canva Pro).
Infographics available for download on the training platform (https://indeed-project.org/)
1.3 Health consequences
The consequences of dysphagia range from compromised general health to more serious problems such as
1.3.1 Security complication
-
Choke: It is the sensation that food is stuck in your throat or chest and it partially prevent air from getting into lungs. It persist breath and start the coughing to eliminate this estrange particle.
How is an airway choke treated?
It is advisable to encourage the person to cough until the element is expelled. It should be avoid drink liquids, eat food or back blows because the foreign object could be fall into airway.
-
Obstruction: An airway obstruction is a blockage in any part of the airway due to a food or foreign object. An obstruction may totally prevent air from getting into lungs that It would be life threatening emergencies that require immediate medical attention.
How is an airway obstruction treated?
Call national health emergency phone number and start with The Heimlich maneuver. This is an emergency technique that may help a person who is choking on a foreign object.
|
Figure 5. The Heimlich maneuver |
Go Video: The Heimlich maneuver |
|---|
|
 Figure 6. Aspiration pneumonia |
|---|
1.3.2 Efficacy complication
-
Risk for malnutrition
Malnutrition is an imbalance of energy or other nutrients (lack of carbohydrates, fats, vitamins and minerals) that causes measurable negative effects on body composition, physical function and clinical outcomes.
The 51% of people with dysphagia are at risk of malnutrition and severity of dysphagia correlates with increase incidence of malnutrition.
-
Risk of dehydration
Dehydration occurs when you do not take in enough fluids, use or lose more fluids than you take in, and your body does not have enough water and other fluids to function normally.
Their consumption is lower due to dislike of this texture or lack of desire to make it, which increases the risk of dehydration.
Dehydration may lead to lethargy, mental confusion, and increased aspiration.
-
Decrease the quality of life
Quality of life may be defined as the degree to which an individual is healthy, comfortable and able to participate in or enjoy life events.
Previous main complications associated with dysphagia may lead to decreased quality of life and social isolation, as well as increased risk of comorbidities and mortality.
All this leads to an increase in dependency, a greater burden of personal and medical care, as well as an increase in institutionalization.
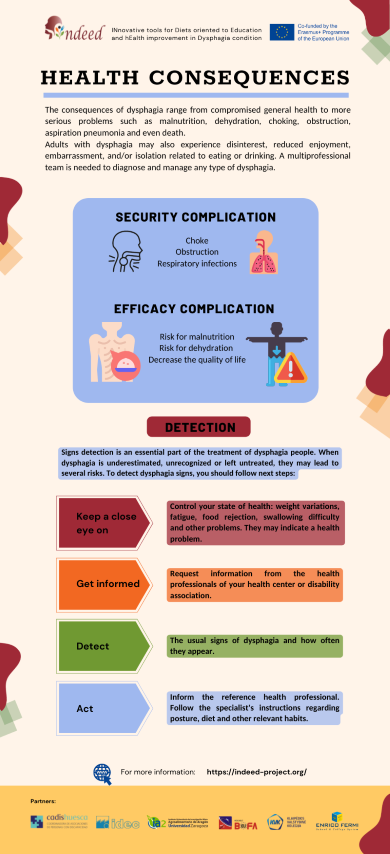
Figure 7. Infographic of health consequences and detection (Source: designed by Canva Pro).
Infographics available for download on the training platform (https://indeed-project.org/).
1.4 Detection and diagnosis
1.4.1 Detection
Signs detection is an essential part of the treatment of dysphagia people. When dysphagia is underestimated, unrecognized (so-called silent dysphagia) or left untreated, they may lead to previous risks mentioned.
For this reason, training elderly or most vulnerable people in dysphagia and other swallowing complications is essential to carry out a correct treatment.
Training to detect dysphagia signs, you should follow next steps:
-
Keep a close eye on: Control your state of health: weight variations, fatigue, food rejection, swallowing difficulty and other problems. They may indicate a health problem.
-
Get informed: request information from the health professionals of your health center or disability association.
-
Detect: Identify the usual signs of dysphagia and how often they appear.
-
Act: Inform the reference health professional. Follow the specialist's instructions regarding posture, diet and other relevant habits
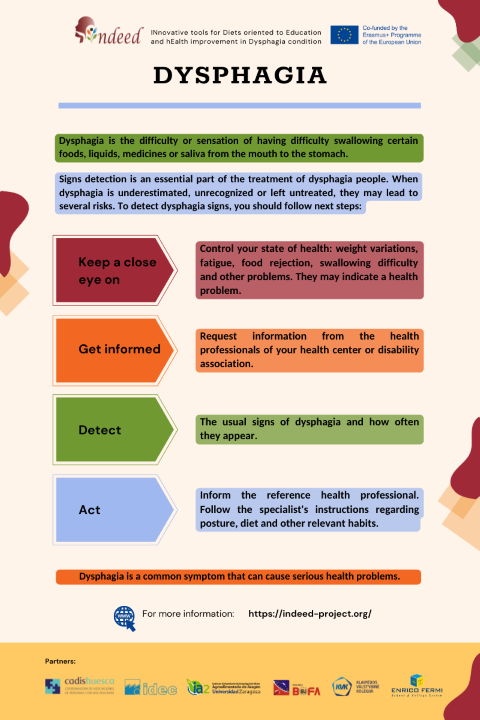
Figure 8. Infographic on the importance of dysphagia detection (Source: designed by Canva Pro).
Infographics available for download on the training platform (https://indeed-project.org/).
1.4.2 Diagnosis
Your doctor can carry out an initial assessment of your swallowing and a physical examination and then refer you for further tests and questions such as:
-
How long you've had signs of dysphagia.
-
whether your symptoms come and go or are getting worse.
-
whether dysphagia has affected your ability to swallow solids, liquids or both.
-
whether you've lost weight.
1.4.3 Treatment and Professionals involved
The goals of dysphagia treatment are to reduce the complications mentioned above. Therefore, a proper diagnosis is essential for a correct treatment and this should be performed by a multidisciplinary team that includes:
Dentist, Gastroenterologist, Neurologist, Nursing, Nutritionist/Dietician, Occupational Therapist, Physical Therapist, Social Worker, Speech-Language Pathologist and others.
1.4.4 Alert protocol
When signs of dysphagia are detected, it is important to start with the alert protocol. The steps of this protocol will depend on whether you belong to a center or association of people with disabilities that has a health area or not.
-
Yes, I belong to a center with a health area. If you detect the repeated presence of suspicious signs of dysphagia, you should inform the health professionals of your center.
-
No, I do not belong to a center with a health area. If you detect the repeated presence of suspicious signs of dysphagia you should go to your nearest health center and inform your family doctor.
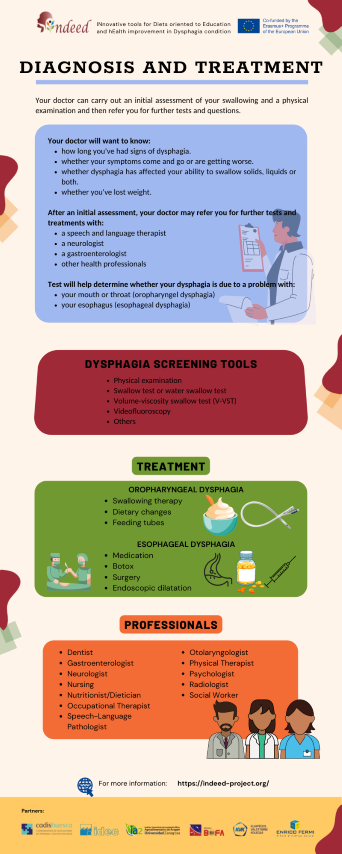
Figure 9. Infographic on the diagnosis and treatment (Source: designed by Canva Pro).
Infographics available for download on the training platform (https://indeed-project.org/)
Resources
https://www.kenhub.com/en/library/anatomy/stages-of-swallowing
https://nrgi.org/EDUCATION/DYSPHAGIA
Sura, l., madhavan, a., carnaby, g., & crary, m. A. (2012). Dysphagia in the elderly: management and nutritional considerations. Clinical interventions in aging, 7, 287.
Https://www.kenhub.com/en/library/anatomy/stages-of-swallowing
Dysphagia
video fluiroscopy: Ianessa Humbert. 8th May, 2020. Normal vs Abnormal
swallowing [Vídeo file].
Explanation
about Dysphagia: CADIS HUESCA. 14th May, 2021. What is dysphagia?
Erasmus+ project INDEED about Dysphagia condition (eng) [Vídeo
file].
Difficulty
Swallowing: FreeMedEducation. 17th May, 2018. What is Dysphagia
(Difficulty Swallowing)? [Vídeo file].
Teasell r et al. Dysphagia and aspiration following stroke. Ebrsr. March 2018 https://www.healthline.com/health/pneumonia#symptoms
Https://www.healthline.com/health/airway-obstruction
The
Heimlich maneuver video: Howcast. 21st
September, 2012. How to Give the Heimlich Maneuver I
First
Aid Training [Video file].
Epinephrine
treat video: NationwideChildrens. 23th November, 2011. How To Use an
EpiPen [Video file].
Speyer r., baijens l., heijnen m., zwijnenberg i. Effects of therapy in oropharyngeal dysphagia by speech and language therapists: a systematic review. Dysphagia. 2010;25(1):40–65. Doi: 10.1007/s00455-009-9239-7
https://www.malnutritionpathway.co.uk/dysphagia.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6302767/
https://www.asha.org/practice-portal/clinical-topics/pediatric-dysphagia/dysphagia-teams/